More Posts from
Gut Microbiome & Digestion

Meet Your Microbiome: The Human Microbiome and How to Optimize It
Meet Your Microbiome: The Human Microbiome and How to Optimize

Benefits of Probiotics Including Improved Gut Health
Benefits of Probiotics Including Improved Gut Health “Probiotics” has become
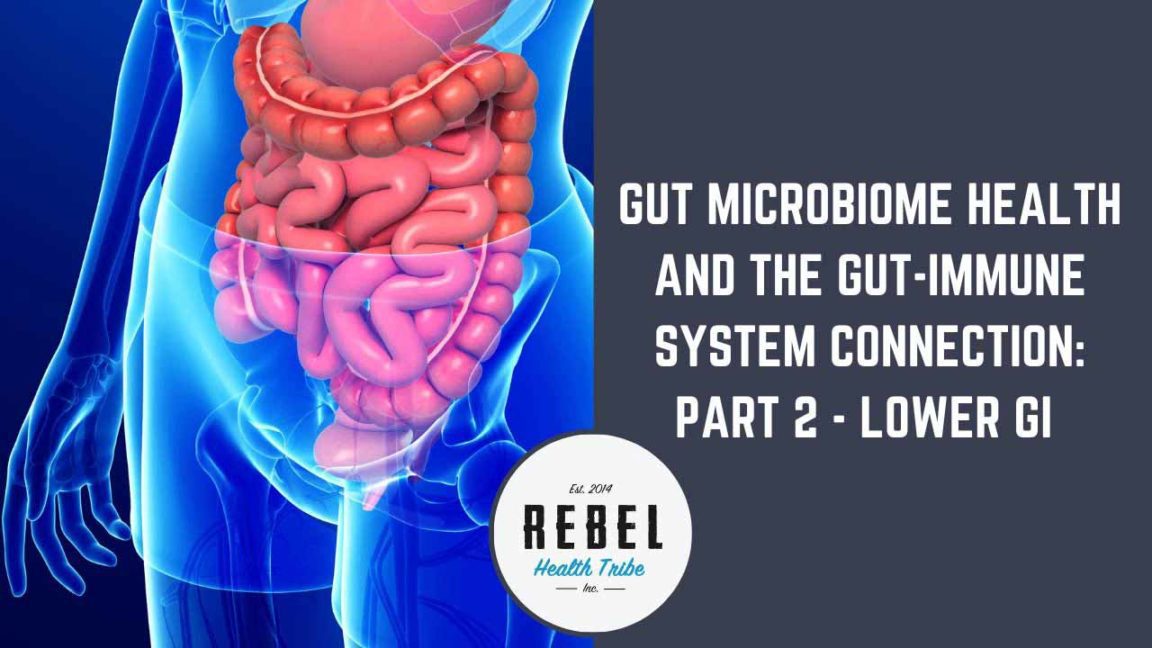
Gut Microbiome Health and the Gut-Immune System Connection: Part 2 Lower GI
Gut Microbiome Health and the Gut-Immune System Connection: Part 2
https://vimeo.com/392771118/
Transcript
Michael Roesslein:
We are back recording. All right. So let’s officially start. Hello, I’m Michael. I’ll be your host. I am here with Kiran Krishnan from Microbiome Labs. Welcome back.
Kiran Krishnan:
Thank you. it’s good to be back. It’s been, I can’t remember how long now.
Michael Roesslein:
I think a few months.
Kiran Krishnan:
A few months, yeah.
Michael Roesslein:
I think a few months. So holidays happened, more travel happened. Where’s your most recent favorite place?
Kiran Krishnan:
I was in Malaysia a couple of weeks ago for a conference there. It’s interesting when you see that part of the world. And I grew up there, obviously, in Malaysia and India, and it’s really nice to see that there’s this swelling group of functional medicine-focused allopathic doctors. Many of the doctors that I presented to and spoke with afterwards work in hospitals. There was a doctor that is a big oncologist there, and he was telling me about the response he’s getting in cancer treatments when he does all of this nutritional therapy beforehand. So he’s doing high dose IV vitamin C, and glutathione, and all this nutritional stuff.
Michael Roesslein:
Before the conventional treatment.
Kiran Krishnan:
Before the conventional, and he’s getting much better response rate, much better recovery rate, and so on. And I’m like, “Wow, that’s amazing. It’s surprising to me that the hospital system would allow this.” And he’s like, “Whoa, they don’t allow it. I’m just doing it on the down low for the patients beforehand.” So it’s great to see that there’s so much conviction in some of these docs and they’re going for it. And they were very excited to have us there really kind of educating them on the microbiome and giving them the latest there.
Michael Roesslein:
Cool. No coronavirus scare in Malaysia?
Kiran Krishnan:
Not at that time. That was right at the middle part of January, about a month ago, so it hadn’t started yet. Next week I’m going to New Zealand and Australia. Or the week after next, sorry. So fortunately, there’s almost no coronavirus there, so all good. Although, we were going to be … Not next week, but the week after, there was a [inaudible 00:02:35] show in Taiwan and that got canceled because of the coronavirus.
Michael Roesslein:
There’s people walking around here on the West coast, in California, with masks. So 3,000 miles is close enough to get a mask on, but I don’t want to make fun. I’m sure there’s people out there who are very scared of it, so I don’t want to trigger anybody.
Kiran Krishnan:
Well, here’s a side benefit that they don’t realize. What’s way more deadly than the coronavirus in the US is the flu, right?
Michael Roesslein:
The flu, yeah.
Kiran Krishnan:
The flu, the mortality rate this year is somewhere around five and a half, 6%, which is higher for the flu normally. Coronavirus mortality rate, even in China, is 2%, so if they’re wearing the masks for corona, at least it’s protecting them additionally from the flu.
Michael Roesslein:
Double win.
Kiran Krishnan:
Yeah, exactly.
Michael Roesslein:
All right. So I just jumped right in and assumed that everybody that’s watching knows us already. So maybe we have some new people on the line that have not watched before. We’ve done about, I don’t know, a zillion webinars at this point, so if you are new, welcome. Kiran is the chief science officer at Microbiome Labs and our favorite resident microbiologist. We’ve done the microbiome series webinars. He was in our microbiome masterclass, the auto immune masterclass, and we do retail a handful of his company’s products in our shop at rebelhealthtribe.com . When we first started doing webinars, we were your exposure to most of the people that were watching, and now they probably see you all over the place.
Kiran Krishnan:
Yeah. Fortunately, yes.
Michael Roesslein:
It’s fun. I see you popping up on friends’ podcasts and websites and interviews, so it’s always fun when I see two of my friends hanging out.
Kiran Krishnan:
I love it. Yeah, Rebel Health has seeded a lot of that, which has been great. And last year I think I recorded about 85 podcast interviews where I was on other podcasts.
Michael Roesslein:
Wow. You need to clone yourself.
Kiran Krishnan:
It’s getting crazy. Today’s webinar, this recording and live that we’re doing is the fourth one I’m doing today. So gone fully crazy.
Michael Roesslein:
Gone full rockstar.
Kiran Krishnan:
Yeah. Full [crosstalk 00:04:56].
Michael Roesslein:
All right. I’m going to set a timer because we have a lot to talk about. So I’m using my phone timer. If you see me on here, I’m using the timer. I am not writing emails or browsing. Before I do that. All right, so we have about a little over an hour, probably hour-ish. So we want to learn about what’s new. I talked to somebody on your staff last week. I talked to [Acacia 00:05:23] and she said, “You’re going to have to ask him because there’s a lot,” and at one point you guys were doing one leaky gut study at the University in Texas with college students eating McDonald’s and MegaSpore, and then the next time I heard there was 12 studies going on simultaneous in different places with different products and combinations and things. And then I just said, “I’m not going to even try to keep track of this. I will just ask him next time he comes on for some sort of summary.” So in the last few months, is there anything that’s either come to completion or publication, or anything that you’d like to share?
Kiran Krishnan:
Yeah, so we do, we have, I think, 19 studies going on right now that are in different phases. They’re either just starting, somewhere in the middle, or almost completed. So there’s a lot of work going on and it’s all really kind of exciting stuff, certainly for us. But most recently, a couple of the things that ended, I think a lot of people saw the publication that came out in August of last year with IBS, and these were IBS-D using a MegaSpore, and the comparison of the effects of MegaSpore when compared to using Rifaximin and a low FODMAP diet, right. So it was a combination of Rifaximin with the low FODMAP diet, and then MegaSpore alone. And what we found was that MegaSpore alone, in this clinical trial, it was a 90 patient, 90 day clinical trial, the MegaSpore alone worked just as well as the low FODMAP diet and the Rifaximin either by themselves or in combination. And in fact, some of the quality of life assessments were actually significantly improved with just the MegaSpore compared to the other therapy.
Kiran Krishnan:
So it speaks to how important it can be for that primary gut issue, which is a irritable bowel. And that’s kind of where everything starts for people that have significant gut problems, it starts with irritable bowel and then it can stem into a SIBO type of a condition, or eventually a inflammatory bowel kind of condition. So, that was a very exciting study for us to publish. Most recently, towards the end of last year, we completed our first acne study, which was submitted for publication, so it’s going through the rounds right now in peer review. We saw a very significant reduction in acne lesion count in just 30 days of taking the probiotic. And this was really exciting because we were getting response from people who send us on social media, our clinicians that send us feedback saying, “Hey, this seems to really helped my patient’s, or my son’s, or my daughter’s acne.” That gave us the impetus to go okay, well let’s study this connection between the gut and the skin, and how changes we’re making in the gut can seem to affect the skin to a point where acne lesion count goes down significantly.
Kiran Krishnan:
And we found that there is a connection with Ruminococcus in the gut and how, if you tend to have low levels of Ruminococcus, you tend to have a higher risk for acne, and one of the effects of adding in MegaSpore is increasing Ruminococcus levels, and that helps clear up the acne. And so now we’re doing a larger version of that study for 90 days. We do have a 90 day, 200 patient leaky gut study that we’re repeating at University of North Texas. Same place we publish our original study. That’s going on. We’ve got a couple of cancer immunotherapy studies starting. We’ve got a rheumatoid arthritis study that is about a halfway through right now that’s really exciting. We just submitted for publication our first dog leaky gut study. We wanted to set out to prove that our canine friends and family have also leaky gut the same way we do. It’s still the same LPS endotoxemia, because the moment we start domesticating dogs into our lifestyle, they start developing things like allergies, and diabetes, and heart disease and all that. Things that you don’t really see in-
Michael Roesslein:
Skin rashes.
Kiran Krishnan:
Skin rashes, atopic dermatitis, things that you don’t really see in canines in the wild. And so to us it became clear that it’s kind of a lifestyle thing. It’s likely endotoxemia. And we did the very first study to prove that dogs have the same type of leaky gut that humans do. And then we created a spore base probiotic for dogs that shows a significant alleviation in endotoxemia, which I’ll talk about today in the product called FidoSpore, which we’re very excited about because not only do we have a love for our canine friends, but there’s all these studies that show that having a dog in your household has significant benefit, not only to the immune system of your kids, and the inhabitants of the house, the incidence rates of allergies, and asthma, and viral infections go way down if you have a dog in your household. And most recently there was a study that came out that showed that having a dog in your household increases your longevity. So it improves our lifespan quite dramatically.
Michael Roesslein:
So I have two. I’m probably pretty close to immortal and invincible.
Kiran Krishnan:
Yeah, exactly. Yeah. You are. Free from allergies and immortal. So what was great to us about it is that dogs have evolved, and I’ve studied the evolution of the canine genus, which is really interesting to see how they evolve from the gray wolf, which is the closest relative of our domesticated dogs, to the type of dogs that we have today. What shifted in their psyche, what shifted in their focus and their instincts, and what we come to find out is dogs are heavily dependent on us, and they focus all their attention on what we are doing, and how they need to create that relationship with us for their survival. So it led us to think that there’s all of these inherent benefits of having dogs in our lives, but at the same time, because we’re bringing them into our disruptive standard American lives, we are also messing them up, and we’re creating all the leaky gut and all this dysfunction in our dogs. So can we resolve that? And that’s why the product FidoSpore came about is we want to fix our canine companions that do so much for us.
Kiran Krishnan:
And we have a number of animal studies. We’ve got studies going on in chickens, in pigs, in fish. I mentioned a second-
Michael Roesslein:
How do you study fish? What are you studying in a fish?
Kiran Krishnan:
So what we’re doing is we’re adding the high carotenoid probiotic to fish feed to increase the color of salmon and trout. Right now what’s happening is the vast majority of these fish come from fish farms, right. And that’s a problem. You want wild caught as much as you can, but still the vast majority of people of the world are eating off of fish farms. The color on these fish are diminishing because the health of the fish diminishes. They’re breeding salmon that looks gray basically, or they’re breeding trout that looks gray, and not the bright orange color and pink color that it’s supposed to be. And that is a direct reflection on, not only the digestive, but immune health of fish.
Kiran Krishnan:
And one of the ways that they combat that is they mix in synthetic [astaxanthin 00:13:06] into the fish feed, or in some cases natural astaxanthin, it’s not always synthetic, but it’s astaxanthin into the fish feed to try to improve the color of the fish. And that is the biggest cost of fish farming. And so we started thinking well hey, we’ve got a probiotic that produces astaxanthin naturally, instead of putting in either this synthetic version or the supplemental version, can we instead use a probiotic to increase the color of the fish? And then it’ll also have all of these other health benefits to the fish. So there’s a company in-
Michael Roesslein:
To make their fish less sick, and less expensive to take care of, and cheaper across the board, and better for people to eat.
Kiran Krishnan:
Better for people to eat. They come with probiotic and immune benefits already, like the fish in the natural ocean. A lot of their color comes from probiotic bacteria in the ocean. And so there’s a big company in the UK that actually does all of these fish studies. They have a tremendous facility with all of these pools where they control every last bit of everything, including the most minute aspects of the water that the fish are swimming in and so on. So we’ve contracted with them to do these studies. So we’re doing a number of human studies, number of fish studies, everything.
Kiran Krishnan:
Our whole concept is that the really important aspect of making us healthy is to improve the health of the things we eat as well. So the chickens, that’s why we’re doing the chicken studies, the pig studies, we’re starting studies with University of Montana on soil and how we can improve the health of the plants by using spore based probiotics in the soil, almost like a probiotic supplement for the plant itself. So overall we’ve got this big vision of improving everyone’s health, not only through direct things that we do for ourselves, but also improving the health of all of the things we eat. So that’s just a quick snippet of some of the studies that are going on.
Michael Roesslein:
Just a quick one, and something that happens since we talked last I believe, was the lab.
Kiran Krishnan:
Yeah, exactly. Oh, [crosstalk 00:15:23].
Michael Roesslein:
Can you tell them a little bit. I saw a lot of pictures on the internet of you holding a large cheque.
Kiran Krishnan:
Yeah. A big fantasy of mine, ever since I became an adult, was to be able to hand somebody a big cheque, for a good cause hopefully. But the idea was that Sacramento State has built this new amazing biological research facility through very generous donations from some of their alumni, and within that facility they’re building out really elaborate laboratory departments, one of which is microbiome focus. They brought in a world renowned professor in that space, Rob Crawford, who worked part on the American gut project and so on. And I know him through some of that research work, and he’s heading up the whole microbiome research area. So the idea is two fold. One is to fund some really intricate mechanistic studies to understand microbial community structures and how influences on those community structures create disruptions in the microbial ecology. That’s very detailed, university type of studies to understand quorum sensing.
Kiran Krishnan:
So we want to dig a little bit deeper into how bacteria talk to one another, and if they are talking to one another, and if we can figure that out, can we understand what they’re saying? Is there a way to interpret what bacteria are saying? Can we intervene and modulate the language to some degree to improve the communication within the microbes? And he’s also an absolute expert in biofilms and everything in the gut occurs in biofilms. So that lattice of communication through biofilms is a really important thing to study. So we’ve got all of these studies that we’ve listed together that we’re funding through Sacramento State. But another aspect of the funding, which we think is extremely important, the funding provides opportunities for even potential new scientists in high school, and certainly undergrads to have projects, scientific projects, studying the microbiome and biological sciences. And so it gives opportunity and exposure, especially to underserved communities, for people to get exposure to basic science.
Michael Roesslein:
That’s awesome. I’m not that far from Sacramento now.
Kiran Krishnan:
Oh, you should pop in and visit.
Michael Roesslein:
So next time you’re in town, let me know if you’re going to be visiting the lab at all and we can come film something.
Kiran Krishnan:
That’d be awesome. I love going there and seeing all the enthusiasm of the young people doing the research work, and it’s super exciting that we’re able to do that.
Michael Roesslein:
Kudos to you man. That’s awesome. And I know that it’s every science nerds dream to have their own lab to play in and design experiments in, and the quorum sensing is so interesting. I’m actually in a training right now where part of the training involves quantum mechanics, and I personally, in my very limited understanding of quantum physics at this point, because I’m not a quantum physicist and you almost have to be to have anything beyond a limited understanding, I wouldn’t be shocked if there was a quantum aspect to the communication of bacteria, because it’s the only thing that can really explain the speed at which these things happen. And even in the body too, they’re starting to think that thoughts and emotions and things like that that happened super quickly, there’s a quantum aspect to it that we can’t measure and don’t necessarily understand because things happen in the body faster than chemical chain reactions can necessarily take place. So I would guess there’s something there. I bet your lab people are going to … It says quorum sensing happens with light, and it’s one of the comments there.
Kiran Krishnan:
Totally, yeah.
Michael Roesslein:
It’s probably photons, right?
Kiran Krishnan:
Yeah. It’s potential quantum entanglement. The whole concept of entanglement.
Michael Roesslein:
Bacteria on the moon, bacteria on earth, communicating.
Kiran Krishnan:
Totally. In a multiverse. We don’t know. I mean they all come from another, right.
Michael Roesslein:
Spores go multiverse.
Kiran Krishnan:
Yeah, exactly. I mean those spores that are present on earth today came from space, the concept of panspermia. And so what kind of information they brought with them here is still for us to discover.
Michael Roesslein:
I’m responding to one thing there. Okay. All right, so I’m going to get to those questions in a bit. Keep putting the questions in the chat. I want to stay on task or else we’ll not get to most of the things. So I have a little question time blocked at the end. Keep putting them in the chat or put them in the … There seems to be a separate Q&A thing, and I have that open too, so we’ll get to as many of them as we can. I’m a little not as adept for navigating the zoom thing yet, so bear with me. Cool. Yeah, I definitely want to go to Sacramento and visit the lab. I think it’s about two and a half, two hours from here. So that’s easy to [crosstalk 00:20:36].
Kiran Krishnan:
Awesome. We’ll plan it next time we go there.
Michael Roesslein:
For sure. So that is the research, the travels, and the lab. There is a bunch of questions … I could ask this real quick. The cats. Were the dog and cat same … People are asking does it work for cats, or is it okay for cats, or is it dog specific?
Kiran Krishnan:
Yeah, they’re spore based, and spores are ubiquitous. They are universal colonizers. There would be no issues at all with cats. We’ve got lots of people that have been using MegaSpore with cats, so we know that’s perfectly fine. So it would be translatable to cats, for sure. We didn’t do the study in cats. We’re not sure if cats have the similar leaky gut. My guess is they do. Cats do not go outside the same way as dogs do, so that may either enhance the leaky gut because they don’t actually go outside and get exposure to other microbes, or it may minimize it because maybe they don’t go outside and get exposure to glyphosate, and Roundup, and all that in people’s gardens as much. So it’s hard to say what is happening with the cat gut in terms of leaky gut and permeability, but the spores are ubiquitous organisms. They are perfectly commensal in the cat’s microbiome, and we know that MegaSpore has been used by lots and lots of people with cats.
Michael Roesslein:
Okay. And the other one that was relevant to the research, have you ever thought to do a study for children with autism spectrum disorder or PANS, PANDAS?
Kiran Krishnan:
Yeah, we’ve been working on conceptualizing an ASD study. It’s a little tough because the end points of ASD are really difficult to nail down. Showing improvement in behavior is a little bit more complex, and there’s so many variable variables because most kids who are on the spectrum have parents that are extremely engaged in their care, and are typically doing lots of different things, right. So anytime you’re doing a study in a subject that is heavily managed with lots of different interventions going on it becomes really hard to [crosstalk 00:22:55].
Michael Roesslein:
Have to isolate the control.
Kiran Krishnan:
Exactly. So the control mechanisms are really tough. We’re conceptualizing just kind of an open label study where we recruit ASD kids and their parents online, and we send them product and then just have them kind of fill out a survey. I’m not a huge fan of those kinds of studies, it’s not hard science, but we may do something like that. I’m a much bigger fan of biomarker studies because, to us, it tells a little bit deeper story. And then that’s the other problem with kids too, is it’s hard to get consent to get blood drawn and so on. It’s a lot harder to go through review boards for that kind of study with kids. Anytime you have to prick a kid or take a venous blood, it becomes a complicated issue.
Michael Roesslein:
Got you. I hope that answers the question. I used to go to Autism … Was it AutismOne? The conference that’s in Chicago. Is that only in Chicago or does that travel?
Kiran Krishnan:
It travels a little bit. In the last five years, I think it’s been in Chicago three of the five years, because I’ve been there in Arizona before.
Michael Roesslein:
Okay. It was in Rosemont when I went, but there was a lot of interesting … Because the people there are very receptive and open to all kinds of different treatments, and therapies, and things. But yeah, you’re right. They’re doing this treatment, this therapy, taking this supplement, doing this diet, this thing, and it switched. So yeah, that’d be tough. But it’d be cool to see just with that open label situation. All right. I’m changing the timer. That is it for that section and now we are on to … I’ll let you choose. We can either talk fish oil, which I’m interested in that, or we could go right into the PhytoSport. We have the two new products to talk about. Whichever one you’d like to talk about first is fine with me.
Kiran Krishnan:
So we put together some slides for it, so I can share some slides, and in the order of the slides, the fish oil comes first. So we’ll just jump into that. Sound good?
Michael Roesslein:
Sure.
Kiran Krishnan:
Okay. Let me share my screen. Okay. You see this?
Michael Roesslein:
Yes, I do.
Kiran Krishnan:
Okay, so let me give people a little bit of background on why this came about in the first place. Of course, anytime we develop a product or look at developing a product, we feel there is some significant need, right. So our motto has been, from day one, if somebody else is doing it really well, it’s not a space we’re going to get into. Even if it’s a really hot area and there’s loads of people buying products in that space, we’re not going to get into that space if somebody’s already doing a great job with it. We started looking at the idea of therapeutic omegas for the gut, and then we started researching is anybody really utilizing omegas in the right way when it comes to gut specific inflammation and health. And we really didn’t find anything out there. And so because of that we jumped in.
Kiran Krishnan:
Now why did we even start looking at therapeutic omegas? Well the reason is when you look at inflammatory cascades that are going on in the gut, a lot of it starts with LPS, which many of you are familiar with, and then it has all of these immune-based inflammatory cascades. So interleukins, cytokines, all of these things, TNF alpha, interferon, gamma, soluble CD14, all of these dendritic cell, macrophage, T-cell driven inflammatory processes that occur both in the gut, in the mucosa, in the lining itself, and then also translates to systemic issues. All of those types of inflammatory cascades drive chronic illness, right. And in fact drive permeability, and dysbiosis, and all that. So that’s why, when we first started, we said we need to tackle that kind of inflammation. That’s where the spores come in. That’s where the IgG comes in, the MegaMucosa, the prebiotic, all of those things help with that kind of inflammatory response.
Kiran Krishnan:
Now there’s a whole other cascade of inflammatory response that has to do with lipid metabolism. And that’s what the arachidonic acid pathway then translates into or differentiates into prostaglandins, and then COX and LOX. And so there’s all of these inflammatory cascades that are driven outside of the immune-based cascades, but are stimulated by the immune-based cascades, right. And this COX and LOX, and arachidonic acid pathway is based on lipid metabolism.
Michael Roesslein:
Hold on. Have you switched sides?
Kiran Krishnan:
No, not yet.
Michael Roesslein:
Okay. Just making sure.
Kiran Krishnan:
No, not yet. Let me switch them and tell me if it switches.
Michael Roesslein:
I just wanted to make sure there wasn’t a visual to go with what you were saying. Okay. No, perfect. Go ahead.
Kiran Krishnan:
Okay, so that’s the important distinction here is that we’ve got the secondary inflammatory cascade that is driven by arachidonic acid differentiation into prostaglandins. And then we’ve got the immune-based cascade, which are driven by inflammatory cytokines, and starting with LPS, which triggers all of it. Now here’s the crazy thing, so that cellular cascade drives and goes throughout the body and wreaks all this havoc, like we’ve talked about many times, but it also stimulates the onset of the arachidonic acid cascade, which is also driven by tissue damage and the presence of immune-based inflammatory cytokines. So then we started looking at okay, we are now dealing really well with this side of the inflammatory cascade. We need solutions for this side, from the lipid side of the inflammatory cascades. And the best things to do that are omega fatty acids, polyunsaturated omega-3 fatty acids in particular, and then all of the components of that is resolved into, right.
Kiran Krishnan:
And one of the things that drives the arachidonic acid pathway is damage, tissue damage. So when phospholipids get released because cells are dying and broken up, that drives this a arachidonic acid pathway. And so we know in a dysfunctional gut you’re getting all of this tissue damage because your mucosal cells are being damaged, your intestinal epithelium cells are getting damaged, and then all of that damage translates into further inflammatory response. So to us it was very clear, for real comprehensive treatment, not only are we doing a good job focusing on this, but we also need the focus on the lipid side of the inflammatory cascade. So I hope that makes sense. That’s how we dove into the omega side, and we said is there a company we can start recommending to people that has the right proportion of omega fatty acids, and the right components that really will help drive the dampening of the lipid base inflammatory cascade, the arachidonic acid-based inflammatory cascade, right? So that’s how I’m going to refer to it for now on is arachidonic acid-based inflammatory cascade.
Kiran Krishnan:
So we didn’t see anyone that had what would be adequate, based on the literature that’s available of the types of omega fatty acids that really support dampening the inflammatory response on the arachidonic acid pathway. So we jumped in and we said we’re going to create our own and provide that as a really, really important therapeutic tool in the whole healing process from gut damage. And this also then becomes a really important tool for mitigating systemic inflammation as well, because the arachidonic acid pathway is one of the biggest drivers of inflammation in the brain, in the heart, in the liver, and in the kidneys as well. So these organ systems are driven heavily by arachidonic acid immune inflammatory activation, right. And remember the immune part of the activation also activates the arachidonic acid pathway. So although we’re stopping that and controlling that, we still have this inflammatory cascade that progresses due to tissue damage.
Kiran Krishnan:
So jumping in, what we started looking at is when you look at most fish oils on the market, they tend to have heavy DHA. And fish oils are broken up into EPA and DHA, and then there’s other components that we’ll talk about, but those are the ones that most people are familiar with, DHA and EPA. Now, DHA got a lot of notoriety because DHA has a lot of impact on systemic response in the body, especially in the brain, right. So DHA became really popular when they started supplementing infant formula with DHA, or prenatals with DHA, because they started to understand that brain and cognitive development is really supported by DHA.
Kiran Krishnan:
Brain and cognitive development is really supported by DHA. So DHA became kind of this, the rock star of the fish or EPA became a little less known. But as it turns out, when you look at the studies, EPA does a lot of the anti-inflammatory work at local sites, especially in the gut, right? So what we see here is reports like this. And when we started digging into literature where short-term treatment with EPA improves inflammatory inflammation and affects colonic differentiation markers and microbiota and patients with UC.
Kiran Krishnan:
So when you start looking at inflammatory bowel conditions, DHA, the brain associated omega really doesn’t do a whole lot in gut associated inflammation. It’s really the EPA. And not only can the EPA bring down the inflammation, but it also affects colonic differentiation markers and more importantly, the microbiota itself.
Kiran Krishnan:
So as it turns out, this fraction of fish oil has a way of influencing the microbiota, almost acting as a prebiotic in a way, right? So it has super interesting affects when it comes to the microbiome officially. And here’s another conclusion. EPA supplementation reduce mucosal inflammation, which is something we talk about a lot. Promoted goblet cell differentiation, which is really important because goblet cells are those important cells that produce the mucin layer. And we’ve talked through the importance of the mucin layer in a number of presentations over the last several years where the mucin layer acts as that really important barrier that keeps the outside world from the inside. And acts as a conduit for translation and communication between the microbiome and the immune cells. Without a healthy mucin layer, you really have a completely compromised immune response in the body.
Kiran Krishnan:
Goblet cells are the cells in the intestinal, because they’re producing mucin and EPA seems to increase the differentiation of these goblet cells. And it also changes the composition of the microbiota. It actually supports the growth of certain keystone strains. So we found that to be quite interesting and we couldn’t find Omega products that had high enough EPA levels when you compare it to DHA levels. Everything seemed to be focused on a higher DHA level.
Kiran Krishnan:
So that was the first thing we started looking at changing in an Omega product is providing higher EPA levels to make it more gut specific. Then the other thing we started looking at something called the AA/EPA ratio. That’s the arachidonic acid to EPA ratio and it’s a very powerful biomarker for inflammation in the body. In fact, huge studies have been done showing that it is a great predictor of all different types of cancers. If you have a high AA/EPA ratio, that means higher amounts of arachidonic acid compared to EPA.
Kiran Krishnan:
Your risk for heart disease, for all types of cancers including most bowel cancers and all that go way up, right? So the AA/EPA ratio is a very important inflammatory marker that is directly correlated with a whole host of inflammatory tissue damage based chronic illnesses. And the way you modulate AA/EPA ratio is to bring up the amount of EPA into the system. And some of the other intermediates that are found in Omega fatty acids. So this one, Omega-3 supplementation was shown to reduce AA/EPA ratio by 40% in eight weeks in elderly people that were depressed. And this is an interesting study, because they were looking at the high rates of depression in elderly people and they wanted to see if the AA/EPA ratio was predictive of that and they found that the AA/EPA ratio was highly predictive of the incidents and the presence of depression in elderly subjects.
Kiran Krishnan:
And then when you gave them the right kind of fish oil, you were able to actually switch that AA/EPA ratio and that correlated with a reduction in depressive symptoms. And same kind of study has been done in cancers and bowel, inflammatory bowel conditions, heart disease and so on. So this became a really important inflammatory marker for us to focus on and the way you go after this inflammatory marker is by having higher levels of EPA in your fish oil.
Kiran Krishnan:
Then the unsung hero in the whole Omega world is DPA. DPA is this really important component of fish oil that actually enhances the absorption of EPA and DHA. And we found hardly any fish oils out there had adequate levels of DPA, if they had any at all, right? And it also specifically provides significant intestinal production. The reduction of the pro-inflammatory cytokine and macroscopic damage, in particular the COX pathways.
Kiran Krishnan:
So the COX pathways are the pathways that lead to Cyclooxygenase production, which results in inflammatory response in cells. If you can inhibit the COX reaction, you result in healthier cells in not only the intestinal lining, but in the gut in general. And then of course all throughout the body as well. And this is one of the things that DPA does, is it plays a powerful role in inhibiting the differentiation of the COX pathway. So DPA is such an important component, especially when we’re thinking about gut repair, when we’re thinking about inflammation associated with gut damage, and we’re thinking about intestinal protection. And then of course enhancing the effect of both EPA and DHA because of its ability to increase the absorption.
Kiran Krishnan:
Here’s just a study protecting D1, which is a type of a PRM, which we’ll talk about the effect of intestinal protection. So we’re looking at all of these fractions of fish oil that are completely underutilized in most of the products, because they’re not formulating this products with the gut in mind and healing from gut type of damage in mind. They aren’t adding in these protections and resolving things that are PRMs that are pre-resolving mediators, which we’ll talk about. And they’re not adding in the important components like DPA and they certainly don’t have the higher EPA levels as well.
Kiran Krishnan:
So what are these PRMs? Well PRMs are pre-resolving mediators. Pre-resolving mediators are found at small levels in most fish oil products. So they’re there, they’re present, but the levels are quite small. In order for them to have the clinical effect, you have to have certain confirm levels of PRMs in each dose. So when you look at Omega fatty acids, the EPA and DHA that you’re familiar with, or even the DPA that you’re familiar with. Before they can actually slow down and stop the inflammation, they are resolved into these intermediate Omega acids, the names of which are here, which we’ll go over in a second. And those intermediates and then the final Omega fatty acids that they’re resolved into are the ones that actually do the cellular action.
Kiran Krishnan:
And what’s important about these is they resolve the normal inflammatory process. So what’s going on is you’ve got to have the ability to convert EPA and DHA into their pre-resolving mediators in order for them to have the anti-inflammatory effects. Bringing in PRMs into the formula stokes that resolution affect and starts to stop the anti-inflammatory response that you get from Omega fatty acids even before your EPA and DHA can be resolved further.
Kiran Krishnan:
So hopefully that makes sense. So you start with EPA and DHA and then there are enzymes that drive the resolution of them into these types of compounds. So PRMs, the pre-resolving mediators, these are hydroxylated metabolites of EPA and DHA. And then when you have PRMs, they drive the formation of something called SPMs, which are the final resolving mediators. These are things called resolvers, protectants, medicines and so on. These are final metabolites of PRMs. So if you imagine EPA and DHA starts up here, in order for them to exercise their anti-inflammatory affect, they have to end up here-
Michael Roesslein:
On the bottom?
Kiran Krishnan:
On the bottom. These SPMs as you’re familiar-
Michael Roesslein:
I’m familiar with them. Mira takes them for inflammation from-
Kiran Krishnan:
Oh okay, perfect.
Michael Roesslein:
Metagenics is like a super high dose SPM product that’s extraordinarily expensive.
Kiran Krishnan:
It is, these are [crosstalk 00:41:05] per month.
Michael Roesslein:
So it is, the practitioner price that I pay for it is more than the retail of anything else she takes, so.
Kiran Krishnan:
Yeah, and they’re so important, they’re hard to come by. And they’re hard to isolate because they tend to be at really low levels in your general fish oil. So they have to be [crosstalk 00:41:23]-
Michael Roesslein:
So then you need like this much fish oil to make that much.
Kiran Krishnan:
[inaudible 00:41:26].
Michael Roesslein:
So what did you … Which the PRMs are what’s added here, which then leads to more metabolism of the SPMs naturally?
Kiran Krishnan:
Exactly. So the PRMs are one step above the SPMs-
Michael Roesslein:
Got ye.
Kiran Krishnan:
… which means that when you take this type of fish oil into your system, you don’t have to wait for the anti-inflammatory effect to come from all of the steps involved in breaking down the EPA and DHA into PRMs, and then eventually SPMs. You already have PRMs there to start stoking the resolution cascade so that you get quicker to the SPMs.
Michael Roesslein:
Faster more efficient.
Kiran Krishnan:
Exactly, yeah. It’s a turbo boost if you will for the anti-inflammatory effect. And a lot of this effect is very specific to localize in the gut and then the local immune system, the mucosal immune system, the intestinal lining and so on. So we didn’t find any products on the market that had standardized PRMs and especially when you combine it with the higher level of EPA and then the addition of DPA, all of which goes together to create this super product for dealing with the arachidonic acid cascade issue that inevitably occurs in the gut. So that’s the Mega Omega.
Kiran Krishnan:
Again, we saw a gap in, we’ve got the cellular inflammatory cascade, which kind of starts off everything, the LPS, the CD14, all of those things, the macrophages and dendritic cell activation that occurs. We’ve been dealing with that through the megaspore, the MegaMucosa, the IgG. That addresses this side of the issue quite well. But then this side of the issue does also trigger this side and so does tissue damage triggers this side, which is the arachidonic acid pathway.
Kiran Krishnan:
We knew we had to create a solution to deal with the arachidonic acid pathway as well, and then we didn’t find anything on the market that really addressed it well enough, because nothing had a high enough EPA, nothing used the DPA enough. And then we didn’t find anything that had standardized PRMs in it to really enhance that resolution. So you get your SPMs without having to spend $150 a bottle retail.
Michael Roesslein:
Yeah, it’s crazy town. I don’t see DPA listed on most fish oil products.
Kiran Krishnan:
They don’t use it. Yeah, it’s shocking to us, because when we started looking at, we break down and we go knee deep into the science and we started looking at all the research and all the components of Omega fatty acids, and you can find so much amazing work done on DPA and people just don’t add it. To us it just doesn’t make sense. So we put it in there and the PRMs, and the higher amount of DPA. So this becomes a very gut specific fish oil and it targets a whole side of the inflammatory cascade that seems to occur in the gut that has all kinds of damaging effects systemically.
Kiran Krishnan:
So that’s the Mega Omega, and it’s … And we partner with a company that gets all of their official oil from Norway. We know the company well. In fact, Tom had been working with this company in his practice for the last 15 years. So we know them really well. We know the CEO and the founder of the company quite well. So we feel really good about the source. Because the problem is, a lot of fish oil actually comes out of Chile and China, right? So most people don’t really realize even some things that say Norwegian fish oil, it could mean that the oil itself is actually coming out of anchovies and sardines and all that that are farmed in Chile or in China. And then may go through a single processing step in Norway before coming here. And then they slap on the Norwegian fish oil label, right?
Kiran Krishnan:
So we dug into that over a number of years, looking at how do you get actual Norwegian caught fish and just utilize that and make sure that your supply chain is not coming from fish farms in these other areas that can be quite contaminated. That’s where the high mercury levels and all that kind of stuff comes in. So we’re very excited about this product and we’re doing, we’re initiating a study on it right now, looking at people with inflammatory conditions and looking at the response, so the AA/EPA ratio using our Mega Omega product.
Michael Roesslein:
Cool.
Kiran Krishnan:
So that’s exciting. And then we’ll talk about-
Michael Roesslein:
I have two questions before we go. I want to ask the question on that product before we jump. So one, you said you know the source, you know the company. Do they do any testing for purity on the omegas?
Kiran Krishnan:
Yeah, that’s a huge part. We put that into the contracts, put a lot of language into that into the supply contracts from them. Because one of the things, one of our hesitations with fish oil is the peroxides and the-
Michael Roesslein:
That’s why I’ve rarely ever recommended them, because 90 plus percentage of them on the market are pretty-
Kiran Krishnan:
They’re oxidized.
Michael Roesslein:
Rancid.
Kiran Krishnan:
Yeah, they’re rancid. And that’s a big problem. That’s a big issue. A lot of that has to do with the processing. A lot of it has to do with the conversion from the ethyl ester to the triglyceride form. The types of solvents that they’re using in that process. Are they using molecular distillation, are they using a different type of distillation process. And then all throughout the production steps, are they checking for all of the lipid peroxides, not just looking at one or two main ones. There are 13 or 14 different lipid peroxides that you can look at.
Kiran Krishnan:
So we were very careful going through this to ensure that whatever is available to us now in terms of technology of analyzing oils and the peroxides associated with oils that we’re utilizing it to really ensure that the quality of the oils and the load and no peroxide levels. So the rancidity of fish oil was a big issue. And then in fact I don’t take a fish oil supplement at all. I never really have for that reason.
Michael Roesslein:
Yeah, me neither. Occasionally I’ll once in a while, but for the most part it’s not something I always would. So how quick does EPA act to reduce inflammation? I saw a couple of comments in there and I don’t know where they got it from. But I have a couple of comments in there from people who already started with the Mega Omega and said that within a few days they noticed a difference who had GI inflammatory conditions. The formulation kind of speeds the effectiveness, because fish oil? My understanding of it was always a more of kind of a cumulative effect that builds up over a little bit of time.
Kiran Krishnan:
Yeah. Which is true for most fish oils, especially when you’re looking at the DHA heavy fish oils, because that has to accumulate in the cells in the brain and so on over time for it to have its effect. This one’s going to be different. It’s going to be a little bit more acute. A lot of it is driven by the DPA, which enhances the bioavailability of EPA and DHA. And then it’s also driven by the presence of the PRMs, which are already going in there and stoking the anti-inflammatory effect right off the bat, right. Without having to rely on the resolution of EPA and DHA, which can take some time. So the way we formulated it, we expect people to see noticeable effects within a relatively short amount of time. It’ll depend on the person in some degree, but certainly it will be shorter than any other fish official that they’ve tried.
Michael Roesslein:
And then the last one. Because of the immune modulation of EPA, the downregulation of those things. Can high EPA have any negative side effects longterm? Is this something more of an acute use situation for people with known inflammatory situations? Would it be something to kind of pulse? Because fish oil, my understanding of it again, I stayed away from it mostly just because of the rancidity of it and I lack of a need for it. I did take some high DHA stuff in the past because I have brain issues and history of concussions and I’ve kind of played around with every single thing that exists that is for the brain. But long-term use of high dose EPA. Is there any concern there with the ongoing immune … Not suppression but downregulation of.
Kiran Krishnan:
No, because it’s a constant battle. So there’s a constant battle with Omega 6 and arachidonic acid type of production in the gut and in the mucosal immune system, and then the balancing of that ratio, the AA/EPA ratio. So there’s no issue with long-term use. In fact, long-term use will maintain a balance of that ratio, which is really what’s critical. And you see that in the elderly and that’s why they’re starting to do more and more studies on the AA/EPA ratio in elderly and how that correlates with things like senile dementia, how it correlates to GI disturbances.
Kiran Krishnan:
In the case of the study we showed you, it correlates with depression, macular degeneration and eye health. All of those things are correlated with long-term disproportion of AA/EPA. There doesn’t seem to be any risk in having a higher EPA, much higher EPA to AA ratio for longterm. And in fact, in my view that’s probably one of the important things to maintain throughout life. Because we’re going to get continuous die off of cells that release more phospholipids. Those phospholipids go into the arachidonic acid pathway. We get lots of Omega 6 polyunsaturated fatty acids, which differentiate into arachidonic acid into our system. And then we’ve got the cellular immune system that’s always trying to trigger the arachidonic acid pathway. So it’s about maintaining constant balance in that pathway.
Michael Roesslein:
Okay.
Kiran Krishnan:
Yeah.
Michael Roesslein:
Cool. That’s all I got. So go ahead.
Kiran Krishnan:
Yeah.
Michael Roesslein:
We’re only five, seven minutes behind schedule, not too bad.
Kiran Krishnan:
Oh, that’s not bad for me. So FidoSpore, I talked about earlier why this is so important. Of course having dogs has all kinds of benefits for our health and our microbiome. And then they’re dependent on us completely. And because we brought them into our kind of a toxic lifestyle they are suffering from significant amount of leaky gut and all that. So we have two papers in peer review right now for FidoSpore, and it’s the first probiotic product designed to address leaky gut and LPS endotoxemia in our fur friends.
Kiran Krishnan:
This is the study set up. I’m not going to go through that, but we looked at two different sets of dogs. We looked at normal dogs, because one of the things we wanted to ensure, which is what I wish every company would do, is that as you’re going into studies, we knew that this product was safe for dogs. But we wanted to see what happens in normal dogs, you know. Is there an effect in normal dogs? Is there any negative effects in normal dogs? So we split the study into two studies. One where we did the study on normal dogs and ones where we selected dogs with known dysbiosis because they were having GI symptoms, right? Some of these dogs were having diarrhea and other GI symptoms.
Kiran Krishnan:
So the results were really quite profound. And we found in a short period of time, this was I think over 31 days. So about a month of supplementation of FidoSpore, we saw a 20% significant, statistically significant reduction in LPS in healthy dogs. So even healthy dogs like humans that are considered healthy normals by the FDA standard have constant influx of LPS into the system. And the LPS is biologically active, meaning it is triggering systemic inflammation and leading to skin disorders and allergies and all these other things that we see.
Kiran Krishnan:
So even in the healthy dogs, meaning non-GI symptom dogs, we saw a significant reduction in the amount of circulating LPS by using the FidoSpore. But then when we would go to dogs with known dysbiosis, these are dogs that are having GI and bowel problems. At the moment we saw 45% reduction in 31 day period. We didn’t change anything about the dog’s diet or behavior, or lifestyle, or environment, but we still saw a statistically significant reduction in LPS.
Kiran Krishnan:
This correlates quite well to the 65% that we see in humans in our first weekly gut study. So it’s quite interesting. The data is quite profound. We also found an increase in the digestibility of the food in both the healthy and in the dysbiotic dogs. So not only are we’re reducing, we’re sealing up the dogs leaky gut, we’re reducing the LPS translocation, we’re reducing all of the inflammatory, systemic inflammatory responses associated with LPS circulating in the dog’s system. But we’re also improving the dog’s ability to digest and assimilate the food that they’re eating.
Kiran Krishnan:
So that was another really interesting finding as well. And we’re super excited about this because there isn’t another probiotic on the market where we want to set the gold standard in our canine probiotics. And of course hopefully at some point we’ll study it in felines as well. But that is FidoSpore in a nutshell. So two papers we’ll be publishing on FidoSpore, and then hopefully we’ll have one study completed by the end of summer on Mega Omega and some interesting aspects of that.
Michael Roesslein:
Cool. 45% reduction in LPS with dogs is pretty impressive.
Kiran Krishnan:
In 31 days, you know, just supplementation. So imagine if you start adding in some better foods and healthier environment for the dogs. You could do all kinds of improvements in the dog’s health.
Michael Roesslein:
Cool. And all right.
Kiran Krishnan:
Oh, how do you get the supplement in dogs?
Michael Roesslein:
Yeah there it is. Yeah, it’s in a capsule or is it a powder?
Kiran Krishnan:
It’s in a capsule. We also added like an liver extract into it, so it smells good and it’s attractive to the dogs. In fact, you’ll find a number of dogs that if you just hold the capsule out in your palm, they’ll just eat it out of your hand because they love the smell of the liver. Now, if they don’t eat it out of your hand, you can always just pull open the capsule and sprinkle it on their food. That’s the best way to do it.
Michael Roesslein:
Okay, yeah. Well that’s what we’ve been doing with the MegaSpore with ours. We just open it and sprinkle on the food. Somebody said a 100 pound dog gets how much? It probably wouldn’t really vary that much, right?
Kiran Krishnan:
It doesn’t, no. Just like humans, whether you’re a 400 pound human or you’re an 80 pound human, your microbiome is essentially your microbiome. There’s no real difference in how you dose things for the microbiome of varying size humans, is same thing with dogs.
Michael Roesslein:
Okay. I was answering questions so I might have missed this part on the FidoSpore, but there’s an additional bacteria-
Kiran Krishnan:
Yes.
Michael Roesslein:
… that is not in the human products.
Kiran Krishnan:
That’s not, it’s called [crosstalk 00:57:18]. Yeah. It’s called pediococcus acidilactici. I started working with this bacteria about eight years ago. And I was introduced to it by a researcher in New Jersey, who was doing studies on atopic dermatitis in dogs and using pediococcus. Pediococcus is really interesting because it’s a also ubiquitous organism found in grasses typically. Dogs are naturally running and sniffing and eating grass. And that to me made a connection, because my dogs, when they have GI upset, one of the things they do is they go and eat grass, right? And that may be your connection there with the pediococcus, because it’s found abundantly in grasses. Pediococcus survives the gastric system pretty well similar to spores and then has a really powerful immunomodulatory effect. The studies that the researcher in New Jersey was doing when he isolated the pediococcus was looking at responses to atopic dermatitis in canines, and the responses were really dramatic.
Kiran Krishnan:
He had examples of dogs who had basically no hair because their skin was so inflamed they couldn’t grow their coats in large parts of the body. So on the back, I still remember this picture that he showed me on one of his PowerPoint of a dog sitting there, just kind of looking depressed and 70% bald on their skin, on the surface. Because their skin was so inflamed from atopic dermatitis they couldn’t grow their hair. Then several weeks of supplementation with this particular strain. And then you see the second picture of this dog looking all happy and full thick coat that the dog was able to grow. So that always resonated with me, and in my mind I had flagged it where if I ever look at developing a dog based probiotic, I’m coming back to this strain, because the effects that he was showing was quite phenomenal.
Kiran Krishnan:
So we had to put that in there for the immunomodulatory part so that it covers a gamut of issues that we see with dogs. The most common health issue in dogs in the U.S. is atopic dermatitis. So we wanted to make sure we’re addressing that. We weren’t sure if the spores addressed that on their own. So we put the pediococcus in there and then we know the spores are going to address all the gut associated issues.
Michael Roesslein:
Okay, that makes sense. Okay. That section was ahead of schedule. So now we are back. We are back. We are only two minutes off my ideal optimal pace and we have … Can you do about 10 minutes, 15 of questions?
Kiran Krishnan:
Sure, yeah.
Michael Roesslein:
I think that would actually get to them all.
Kiran Krishnan:
Okay. And then do you want to go to buy a [inaudible 01:00:10]?
Michael Roesslein:
Oh yeah. All right. Let’s do, I knew there was a reason we were ahead of schedule. Let’s do that. Let’s answer a couple of questions and then we have a cool announcement and something to talk about at the end. That is going to be the testing.
Kiran Krishnan:
Yeah.
Michael Roesslein:
I only have a few questions here, so I don’t know what Taheebo tea is, but somebody asked, “Is it okay to use Taheebo tea while taking MegaSpore?” Are you familiar with that?
Kiran Krishnan:
I’m not. No, no.
Michael Roesslein:
All right. Sorry. I know you guys have a protocol that you share with practitioners around C diff. Can you share that here or is that something that needs to be sent out?
Kiran Krishnan:
Yeah, I can tell you what we recommend them doing, and again, if you have C diff or you suspect you have C diff, go to a doctor [inaudible 01:01:01] out, it can be dangerous so don’t just treat yourself. But what we recommend doctors look into is either supplemental treatment to other things that they’re doing or however they want to decide with their patients is we do two MegaSpore in the morning, two RestorFlora in the afternoon and two H258 in the evening. Now that order can be switched. It doesn’t seem to matter, but the two, two and two seem to be really important and effective when it comes to C diff issues.
Kiran Krishnan:
And a lot of that is if you have active infection going on, you should probably be in the hospital getting that treated. If you have constant bloody diarrhea, that’s not a time for you to be looking at this. The idea is for people that tend to have recurrence, for people that have had a C diff bout, but then it keeps kind of coming back to some degree. Over time the question has been, how do you keep it under control to some degree in your gut, because it never is completely gone. That’s where this protocol comes from.
Michael Roesslein:
Okay. [inaudible 01:02:12] tea, are you familiar with that? People use it for-
Kiran Krishnan:
Oh, [inaudible 01:02:16].
Michael Roesslein:
No, that’s a different one. That’s a whole nother question.
Kiran Krishnan:
Okay, the cat claw?
Michael Roesslein:
Yeah. Would that cause the MegaSpore to be less effective as it kill the spores?
Kiran Krishnan:
It wouldn’t, no. We’ve tested the MegaSpore against a number of antimicrobials, including biocytin, which is a very potent one. We’ve actually incubated the spores in the biocytin for a period of time and found them to be perfectly stable.
Michael Roesslein:
Wow, that’s impressive. That stuff almost kills me. Let’s see. Is the EPA and Mega Omega in triglyceride form or in phospholipid form?
Kiran Krishnan:
It’s in triglyceride form.
Michael Roesslein:
Okay. Difference between pro- and pre-resolving mediators.
Kiran Krishnan:
Yeah, so the pre-resolving mediators are the PRMs.
Michael Roesslein:
PRMs yeah.
Kiran Krishnan:
The pro-resolving are the-
Michael Roesslein:
SPMS at the bottom of the equation, yeah.
Kiran Krishnan:
So the pre become the pro.
Michael Roesslein:
Yeah, yeah. Pre become the pro. All right. All right. That’s all I got right now. Let’s do it. Let’s talk about the BiomeFx and you’ve got some questions to answer. Because you’ve come on these webinars before and told me you don’t like stool testing very much and that there’s huge flaws with it and that the current stool testing wasn’t very usable and it caused an uproar. And I got lots of angry emails. And I had practitioners reaching out to me saying, “Why are you putting this stuff out there, because I use those tests in my practice.” And I say, “I don’t have a practice. I just share information, so sorry.” So you’re in trouble with some people.
Kiran Krishnan:
Yeah.
Michael Roesslein:
And I would like you to back up your decision to do this.
Kiran Krishnan:
Yeah.
Michael Roesslein:
And share with us what the deal is. So BiomeFx is a stool test.
Michael Roesslein:
Biome FX is a stool test technology or stool test that you guys have worked with a lab to create. And I know a little bit, but I don’t want to butcher it, so I’m going to let you just go ahead and we’ll get into that for the last time that we have.
Kiran Krishnan:
Yeah. And so the development of this has been quite reluctant on my side. And to be honest, I don’t, and I never did like stool tests, what was being offered on the marketplace. And my recommendation to most people was, just don’t do them. Because I get just hundreds and hundreds of emails and messages from people on Facebook and Instagram and all that. A lot of times sending me their stool test reports confused as hell as to what it means. Worried in most cases because they see this arbitrary organism is high, what do I do about this one high organism? Well, we don’t even know if any of that information is actually accurate. Right? And so my rally against stool tests is still what I would do. And so ’til today, most of the stool test on the market don’t really afford any sort of useful practical information.
Kiran Krishnan:
And more often than not, in my view, they mislead people and they cause confusion in the therapeutics. And sure, granted, I know lots of practitioners who use it, who use them and use them as a guide. And, but that’s not the only thing they’re doing. Right? They’re using organic acid testing, immuno testing and all of that stuff. And hopefully they’re good practitioners that take a really strong history and so on. So a lot of times people will say, “Well, I use the those stool tests and they really help.” And then when I dig down deeper and go, “Okay, tell me something in this patient’s stool tests that really kind of guided your therapeutics.” And oftentimes it becomes hard for them to explain what was there. A lot of times it just comes to, “Oh, we saw these pathogens were high. So we did antimicrobial therapy for X number of months and it seemed to improve things.”
Kiran Krishnan:
Well more than likely they would’ve done that anyway because that’s kind of the approach that a lot of people take. Right? The whole idea of kill and recede, kill and recede has been a really staple part of the functional medicine community for a long time. Whether you do a stool test or not. The technology behind most of the stool tests is antiquated. This is like 20 year old technology. The 16S sequencing, it is inaccurate at the species level. There’s no argument about that in the scientific community. Everybody who’s involved in genomics, metagenomics, any of the O-mic’s agree that 16S is not adequate to identify bacteria to the species level. So, we know that all of those tests that are using 16S technology, which the vast majority of the most popular tests are, they’re not adequately or accurately identifying bacteria to the species level. Right?
Kiran Krishnan:
And if you don’t identify bacteria to the species level, then how valuable is your test to begin with? And then let’s assume you can identify bacteria to the species level. What kind of information are you giving people? What are you looking for within the test? The thing that bothers me the most with many of those tests is it gives you the list of organisms and tell you high or low, right? What does any of that mean? Because here’s a true thing about the microbiome. When you look at the presence of any single bacteria, the presence of that bacteria is not as important as understanding what else is present around that bacteria.
Kiran Krishnan:
The microbiome is a very complex ecological structure, meaning there are intertwined effects within all of the microbes that exist in the microbiome. So, the presence of any one given microbe, whether you’re you’re pointing it to be a high or low, is not as profound as understanding of the context of the presence of that microbe.
Kiran Krishnan:
So, the mapping, the ability to map the surrounding community and the relative abundance of the one microbe that you’re testing is really critical. So, that whole aspect is not found in most of the stool tests out there because that kind of ecological mapping of the microbiome is a very specialized science that is really headed up by one individual or group that they tend to work with. And we’ll talk about her in a second.
Kiran Krishnan:
But that was another confounding issue that we found is the 16S technology’s just inaccurate. It’s not giving you accurate species level information. And then on top of that, what they’re telling you about your microbiome is not really actionable, right? It’s not functional. It’s not telling you anything about the function or dysfunction of your microbiome. You’re getting highs and lows of 30 or so bacteria that they tend to test for. So, all of those things really irked me and I got hundreds and hundreds of emails from people and messages about problems they’re having trying to interpret and understand their stool tests. And so are-
Michael Roesslein:
Hold on. Do you want to take off your screen share or do you have other stuff to put up?
Kiran Krishnan:
I have other slides on here.
Michael Roesslein:
Okay. Cool. I just wanted to make sure.
Kiran Krishnan:
Yeah. So, but here’s the reality, in talking to people and talking, and we have tens of thousands of practitioner clients who seek patients and clients all the time. And across the board, the response is, patients want to do the stool tests, right? People love to do and see the tests. They want an understanding of what’s going on in their gut. It’s an intangible place. You know, if you have a rash on your hand, you could see it. You could see it changing and progressing over time. If you have a cut somewhere, you could see it. You could see the damage, you could see the healing happening. The gut is intangible. You can’t go in there and look and see what’s happening. So, people wanted some form of a test, so they’re more connected to what’s happening in their microbiome.
Kiran Krishnan:
And so it became very clear to us, even though we’re telling people, “Just don’t do those tests.” That they’re still going to be doing them, right? And then people started poking at us and going, “Hey, you’re microbiome labs. Why don’t you come up with a better test?” So we started saying, “Okay, is there a way to do a better, more accurate stool test? We’re not going to go with a 16S technology.” Which I’ll show you a slide on in a second. So, what is the other available technologies? There’s something more advanced and as it turns out, there’s something called whole genome sequencing. It’s been around for some time, but the problem with the whole genome sequencing, because you’re looking at the entire genetic map of a bacteria before you identify it, it’s a very expensive to do. 16S is looking at three or four out of six variable regions of a bacteria’s genome to try to piece it together to identify the bacteria.
Kiran Krishnan:
16S is looking at a whole picture, and this is a really important distinction. And I want to give you an analogy that I’ve used before to explain it. So, imagine you take a person, take Michael for example, and we took six pictures of very finite parts of his body. We took a picture of the tip of his nose, one of his shoulder, one of the back of his head, one of maybe his knee and in six locations in the body. And then you show somebody those six pictures and you’re trying to identify Michael from those six pictures. Right? Now, you may be able to look at those pictures and narrow it down that, hey, this looks like a male’s nose or face, so it’s not a woman. So, you eliminate women. Now you only have 50% of the population. This is a white male because you could tell the skin tone, so now you’ve eliminated more.
Kiran Krishnan:
So, you can narrow it down based on what you’re looking at. But can you accurately say that that’s Michael himself, right? And not someone else that is somewhat similar in tone, in face, in hair color and so on. That’s the 16S type of resolution. You can narrow it down to the genus level, but to get down to the species level, you really can’t. Whole genome sequencing is like taking a high risk res of Michael and going, who is this person? Clearly it identifies him with every aspect of his characteristic.
Michael Roesslein:
Don’t get it too high res or you might regret it.
Kiran Krishnan:
But no doubt it’ll be you, right?
Michael Roesslein:
I might look better pixelated.
Kiran Krishnan:
I look good in the dark. That’s why I used to like the clubs. I’m like, ooh, I look good in the dark, in the club. Then the lights turn on. You’re like, oh crap. So, that’s the difference in technology.
Kiran Krishnan:
So, what most people are using right now is a stool test technology that uses those little snapshot pictures of different parts and try to mix it together and make a guess as to what bacteria is there. That drove me crazy and especially because of the prices they’re charging for these tests because the 16S sequencing is really cheap to run, right? It’s 20 plus year old technology. It’s very cheap to run today. So, understanding that they’re charging hundreds of dollars for this type of sequencing, drives someone like me crazy, that tries to provide people with really good value and really practical solutions for the healing. Right?
Kiran Krishnan:
So, we said, “Okay, if we’re going to work on a stool test, we’re going to eliminate the whole idea of 16S. Let’s go with whole genome sequencing. Is there an affordable way to do whole genome sequencing where it doesn’t cost $1,000 a test?” And that’s where we partnered with CosmosID, and I’ll talk about them a little bit more, but they have a high efficiency whole genome sequencing that is affordable and gives you 98, 99% accuracy in species identification, right? So, that right there is a game changer in how you look at what is present in your stool. So, let me run through this a little bit. Let me skip through this part.
Kiran Krishnan:
So, if you can do a high resolution and accurate stool test where you identify specifically the species that you’re finding, and most importantly, if you can accurately map them to the surrounding community in the microbiome and look at true relative abundance. So, you understand not only who’s there, but who else is there and what all of their proportions look like. And then you can map all of those proportions to healthy normal individual’s data that has been downloaded and collected starting with the Human Microbiome Project all the way through the American Gut Project. If you can make those correlations and comparisons accurately, then you might be able to provide some clues. It’s another key.
Michael Roesslein:
We’re still seeing FidoSpore.
Kiran Krishnan:
You are?
Michael Roesslein:
Yeah.
Kiran Krishnan:
Oh.
Michael Roesslein:
I see it within the program. Like within PowerPoint. I’m not seeing a slide show.
Kiran Krishnan:
Oh, okay. Let me-
Michael Roesslein:
I saw it like I was in PowerPoint. Okay, now it’s gone. Maybe just redo it.
Kiran Krishnan:
How about now?
Michael Roesslein:
Yes. Back.
Kiran Krishnan:
We shared.
Michael Roesslein:
Yep.
Kiran Krishnan:
So, now you see a slide that says, “Value of stool testing.”?
Michael Roesslein:
Value of stool testing. Yeah.
Kiran Krishnan:
Okay. So, if you can get an accurate stool test down to the species level, if you can do the mapping effectively, if you have the database of healthy normals that you’ve data mined and mapped and categorized and characterized, and you’ve looked at all of the interactions, the ecological interactions there, and you can correlate that to disease prevalence, then you might be able to give another effective piece of the puzzle when you’re looking at a holistic patient, right?
Kiran Krishnan:
So, it reveals trends within the health and reveals functions and dysfunctions within the microbiome. And I’ll show you some specific examples and it can provide insights into personalized nutrition ideas and nutrition ideas that are more geared towards what your microbiome does with the nutrients versus just taking a guess as to what foods are healthy and not healthy for you. And ultimately it can empower the patient to take their health into their own hands.
Kiran Krishnan:
Because when you have a well done report that is very accurate, that provides actionable steps, you’re providing the individual with an understanding of why these kinds of foods don’t respond well to my body. Why these kinds of foods do really respond well and then empower people to make those kinds of lifestyle changes and judgements that help them kind of take their health into their own hands. Now, there are still limitations. This is not the be all, end all of testing, nor is this the only thing you should do to try to figure out what is going on in your system because it is not a diagnostic tool, right? Stool testing, sequencing are still not approved as a diagnostic tool. It doesn’t have the history of use. It doesn’t have all of the validation used for diagnosing a condition, whether it’s an infection, a disease condition or whatnot.
Kiran Krishnan:
It is not a diagnostic tool. Sampling methods are limited in that when you sample your stool, you’re getting a sample of that snapshot of stool, right? We don’t know if you sample a hundred stool samples a hundred days in a row if there’s going to be in small variations in the microbial population, so we know that we’re getting a snapshot of that time. Now, hopefully if the statistics are done correctly through microbial ecological work, then you’re getting a decent representation of what the microbiome tends to look like. Certainly in the distal colon, but still it’s a snapshot, so you want to keep that in mind as well. And of course 16S versus whole genome. We talked about that and lack of report interpretation, lack of actionable steps, lack of functional analysis within the report is really a big issue within stool testing itself.
Kiran Krishnan:
Here is a, we didn’t put the company names, but here’s five of the leading stool tests. Four out of the five still use 16S. Pricing varies anywhere from right under 300 to close to $600. Most of them use a small scooper. There is one company that uses metogenomic sequencing but the problem we found with them, which is a whole genome sequencing, is the report. The report doesn’t really tell you much of anything. It’s not looking at functional analysis of the microbiome. So, although they likely have the technology to be able to do that, they just haven’t been able to conceptualize that part yet. But these four are the vast majority that people are using. This is still a relatively new one. So, these four represent this old guard technology, the poor reporting, the not giving you any functional analysis and so on.
Kiran Krishnan:
This is a 16S region. I talked about this a lot, but there are these variable regions within the DNA of every bacteria. If you can match all of the variable regions, you can identify a bacteria, but lots of bacteria share similar variable regions. And the question is if you don’t find all the variable regions in the DNA samples, if you find just three out of the six or four out of the six, are you accurately predicting what bacteria that is? And we’re coming to find out that it’s not accurate. Whole genome sequencing is end-to-end sequencing like I talked about. And then at the end of the day, the functional analysis, we’ll go through a couple of pages of the report quickly, because of time, as we’re always going over, just so you kind of understand what we’re looking at and how we’re reporting in data and why this is truly a functional analysis of the stool.
Kiran Krishnan:
And again, this all was reluctantly developed, right? Because we’re not fans of stool tests and we come to understand that people still want to do a test, practitioner’s still want some guidance as to what’s happening in the microbiome. We know diet impacts the microbiome severely. We know your environment impacts the microbiome severely. So, they wanted some sort of guidance to understand what is happening in the gut so they can create their therapeutic regimen for their clients and their patients. And so our response was, okay, we named ourselves Microbiome Labs. We should be the leaders in anything microbiome. If people are going to be spending their hard earned money doing stool tests, let’s develop them the best possible test that the technology allows us to develop right now and offer that into the market. So, that’s where it came about.
Kiran Krishnan:
And of course the most important aspect of what you get from the test is this functional analysis. Now, I mentioned earlier that we partnered with CosmosID for a reason, right? When we started MegaSpore, when we started, sorry, Microbiome Labs and our flagship product MegaSpore, we knew that we wanted to be in the spore space. We felt strongly that spores had a very unique therapeutic effect within the microbiome and of course since launching, we’ve done a number of studies to prove that and have tens of thousands of people that use a product that would provide testimonials that the spores are highly effective. But when we decided to do spores, our initial response was, we got to find the preeminent researcher in spores and go and work with him or her. That’s when we found Dr. Simon Cutting and we immediately formed a relationship and an agreement with Simon Cutting.
Kiran Krishnan:
And we wanted to work with the world’s leader in that space. That’s the same thing with stool testing. If we’re going to look at gut, microbial, ecological factors, we want to work with a leader in this field, and there’s nobody that even comes close to Rita Colwell. Right? So, she’s an environmental microbiologist from the University of Maryland and Johns Hopkins. She was the director, the 11th director of the National Science Foundation, which is a very high esteemed position to have as a scientist. She’s got all of these memberships and what’s really impressive to me is she has over 800 scientific publications, right? You look at your typical career scientist, they will have somewhere around 150 to 200 publications. She has 800 in this field. That is leaps and bounds beyond anyone else in this field. She’s an absolutely amazing juggernaut of a scientist.
Michael Roesslein:
Only 800.
Kiran Krishnan:
Only 800 published papers, including 19 books. Many of these are textbooks on the subject, right? So, this is the pinnacle of knowledge on this subject. She has 64 honorary degrees. Besides the degrees and the PhDs and whatnot that she earned herself, 64 honorary degrees. I’ve never met a scientist with that many honorary degrees. It’s absolutely mind boggling. She has a National Medal of Science from president Bush in 2006 to Stockholm Water Prize. The Order of the Rising Sun gold and silver star from the emperor of Japan. I never even knew that that’s something that was given.
Michael Roesslein:
I didn’t know that most of these things were things.
Kiran Krishnan:
It’s insane, right? It’s insane, and you look at this unassuming sweet looking woman and she is a juggernaut in the world of microbial ecological sciences. National Women’s Hall of Fame. All of these other things, amazingly well decorated, and here’s what’s most important about it. Why we would choose to work with someone like this is because remember the technology aside. Let’s say everyone can do whole genome sequencing and get the most accurate species level data. Let’s say everyone can do that. The thing is when you get sequencing data, you get several terabytes of data from a single individual, right? The ability to interpret that data and make sense of it and correlate it to effects in the body and effects as it’s related to disease is a whole other science. That requires an immense amount of microbial ecology work and Rita is the leader in that.
Kiran Krishnan:
So, even if other companies can do the whole genome sequencing, the interpretation of the data and understanding of the data is a whole other science on its own. There’s nobody in the world that is more qualified than her. Her work and the foundation of CosmosID started with the 2001 outbreak in anthrax and she was recruited to run the inter-agency advisory committee for the FBI and the CIA to develop the strain ID and metagenomics and novel genomic methods to ID the types of anthrax strains that were being used in those attacks that were perpetrated in 2001. And she also found ways of understanding the ecological interactions of anthrax with all of the other microbes in the environment. And so she ran, she headed up the chair, that inter-agency department and then based on that work she started the foundation that led to the formation of CosmosID back in 2008. So, you couldn’t find a more decorated head and company that has a better pedigree to do this kind of work. That’s what attracted us to them.
Kiran Krishnan:
So, that’s why we work with CosmosID on this as a sequencing partner. And then we created all of the different functionalities that we want to analyze. They did all of the mapping and the ecological work to try to figure out how to map those functionalities. So, let me just jump, in the interest of time, a little bit to the report itself. This is someone’s actual report, and I’ll go through this kind of quickly because I’ve recently recorded much more detailed explanations of each section of the report. What it means, how to read the data and all of that stuff, how it connects to other sections of the report. Those videos will become available as well, and Michael has full access to those. So, he’ll be putting those up. So, you can go and you can look at each section of the report and get a whole video explanation from me on what that section means.
Kiran Krishnan:
So, I’m going to give you more of a cursory view on this or we’re going to end up here for another hour just going through the report, right?
Michael Roesslein:
We can do another chat on this in like a month or two also.
Kiran Krishnan:
Totally. Yeah. So, the first part of the report and the way we look at ecosystems, right? Is you first need to look at the broadest characteristics of the ecosystem and then if some of the big, broad things are out of whack, then you’ve got to fix the bigger trends before you dig deeper into the ecology, the ecosystem to really understand what small, minute things need to be adjusted. I gave an example in a recent recording I did. Let’s look at our microbiome as like a town or community, if you will, and the community has to have all different actors in order for the community to sustain itself. And let’s imagine this is an independent community on its own without any other communities around it to support it. So, it has to have all of its own functionality in-
Michael Roesslein:
Your screen didn’t change again.
Kiran Krishnan:
Oh. That’s right. Let me stop and reshare.
Michael Roesslein:
Just so everybody knows on Webinar Jam there is an ability for me to make a sticky post, which everybody could see at all times. We are doing a coupon for the two new products and I keep posting it in the chat but I know not everybody’s watching the chat. I put the link to our shop in there and there’s a 10% off code that works for both of the new products. The FidoSpore and the Mega Omega and it will work until Sunday night. So, it’s a few days. We’re going to get this recording put together and transcribed and sent out hopefully by Friday, definitely by Saturday. But the code is fidomega, all one word, F-I-D-O-M-E-G-A 10, fidomega10, and no capital letters. All one word, fidomega10, in the shop gets 10% off both of those products for the launch for this weekend. So, check out the chat if you want the link. All right. Go ahead. Wow, that’s cool.
Kiran Krishnan:
Yeah. So, you can see the report now, right? The first page?
Michael Roesslein:
Yeah.
Kiran Krishnan:
Okay. Awesome. So, remember with ecosystems, you look at the biggest trends first and then you scale down into more and more finite and specific information. And that’s kind of how the report is laid out. Step one is we want to look at the biggest trends within your microbiome to see how you map to a U.S. healthy population. Now, what is this U.S. healthy population? Well, there is well-established data on individuals that have no chronic illness and aren’t taking any medication to manage any disease. There’s about 460 or so microbiome, full analytics, done complete shotgun, end-to-end sequencing and a company like CosmosID has the bioinformatics capability of getting all of that data and then mining it and going through it and creating characteristics that are common among the healthy population.
Kiran Krishnan:
And the healthy population, is a span of children all the way to elderly women and men about equal distribution because again, the microbiome doesn’t really shift all that much between sexes and between age. Right? The only thing is it tends to get low in diversity as you age, but again, this is a healthy population and we’re mapping all of these trends and patterns against where the U.S. healthy population seems to fall.
Kiran Krishnan:
So, the first part we’re looking at, you get something called your Gut Microbiome Index Score. The higher the index score, the better. It’s looking at a few different things. It’s looking at your alpha diversity, beta diversity, resistome occurrence, and a pathogen control index. I’ll just give a quick snippet on each of those. They add all of that together and give you this score. Now, the score tells you in general how healthy the population of your microbiome is and how well it’s suited for this ecological environment, which is the U.S. Right?
Kiran Krishnan:
Because if you had the microbiome you have right now, like this individual’s microbiome seems to be well adapted for the U.S. Population. If this individual moves to Mexico City for example, that ecology is very different than the U.S. ecology. This microbiome is not well adapted for that population or that that ecosystem. So, all of this is geared towards specificity around U.S. population because the geography matters a lot. So, the first thing is alpha diversity. That is how diverse is your microbiome in terms of the number of species that are found in your microbiome. This is something called a whisker plot that is almost like a bell curve. When you look at the box, the middle box is where the median score is, this is where the average person, U.S. healthy populations diversity will score. This is kind of the top end and this is the bottom end.
Kiran Krishnan:
So, think of this whisker plot, which you may not be familiar with looking at as a bell curve, right? So, this is the bell curve. This gray area will be the peak of the curve. And then this is where the highest diversity is, and this is where the lowest diversity is within the U.S. healthy population. So, this individual is clearly on the higher end. They’re in the upper percentile, high upper core quartile of diversity. So, they tend to have pretty good diversity in their microbiome with regards to U.S. healthy population. And we actually give you the species count care about 148 identified separate species within that person’s microbiome. So, that’s what that’s telling you.
Kiran Krishnan:
Now again, across the board, the higher the diversity, the better in general, right? If your diversity was really low and that’s one of your main ailments that you’re dealing with and your bar would be somewhere down here showing the diversity is either in the lower quartile or even way lower than the typical U.S. population.
Kiran Krishnan:
Now the beta diversity tells you how similar your composition of bacteria is to people that live in the same geographic region. So, this is where everyone in the U.S. The healthy population that has been tested tends to cluster, right? In this particular plot. This person’s sample is right in the middle of the density of the cluster. That means their bacterial composition is very similar to those healthy individuals within the U.S. Now, if yours as clustered way out here somewhere in one of these corners, then you know one of the problems with your microbiome is that it’s not well adjusted to the geographic location of being in the U.S. because you’re clustering quite far away from where the typical healthy population is in the U.S. So, you’ve got species within your microbiome that aren’t typically found in any great amount in the U.S. population. And you’re clustering outside of the norms.
Kiran Krishnan:
So, your microbiome is not well adapted to being in this location. That could come from having just recently moved here from a foreign country. It could come from having spent the last few weeks in the Amazon and getting exposed to all kinds of stuff out there. It could come from taking multiple courses of antibiotics and you’re really dysbiotic. So, that’s what that tells you. And again, in my other video explanations, I go into the meaning of a lot of this and how you interpret some of this stuff a little bit deeper. This is the resistome, the resistome actually looks at, it’s not what most people think. Most people see that and they go, “Oh, it’s antibiotic resistance.” No, that’s not what we’re measuring. We’re actually measuring ecological forces within the microbiome that create competition within the population.
Kiran Krishnan:
Now, in any ecosystem, competition is a good thing. It actually maintains stability in the population. The moment competition goes out, you start to get huge overgrowth in certain populations that are favored by that paradigm. Now, same thing that happens in human ecosystems and animal ecosystems all over the world, right? The moment you take out the resistance from all of the different bacteria, you start to get abberant growth of others. So, what we want to see here is a higher number and this individual, despite having good diversity and mapping, their resistome is a little bit weaker, is a little bit lower, which means that there is some vulnerability to their microbial population, meaning some force that comes in, like a single course of antibiotics could totally throw this diversity off and it could throw off their beta diversity as well. So, this individual would want to work on improving the ecological forces that maintain stability within the microbiome. Then the last thing is…
Kiran Krishnan:
…that maintain stability within the microbiome. Then the last thing is the pathogen control index. What this is looking at is looking in all of these really prevalent pathogens within the US population and looking at their relative abundance to the rest of the commensal bacteria. The presence of pathogens alone doesn’t mean that there’s any issue because most of us have pathogens within the microbiome. Right? That’s totally fine. But it’s the context that’s really important.
Kiran Krishnan:
It’s, what is the relative abundance of each of the pathogens and collectively all of the pathogens compared to the rest of the microbiome? And if the rest of your microbiome is more abundant and has the ability to control their pathogens, you’ll have a high pathogen control index. Which this means in this individual’s case, they have a very high pathogen control index, which means whatever problems they may or may not be facing are not likely due to any pathogens within the microbiome.
Kiran Krishnan:
So, they don’t need to think about antimicrobials, they don’t need to think about targeting pathogens. That shouldn’t have to be part of their healing and therapeutics. The resistome may be an issue, but the pathogen occurrence is not. So, that gives you your first view of the overall picture of your microbiome. Is your diversity okay? Do you have the typical composition of bacteria? Are your ecological forces strong enough to resist aberrant growth of certain microbes within your gut?
Kiran Krishnan:
That tells you the resilience of your microbiome. Can you get exposed to a single course of antibiotics and bounce right back? Or because your resistome is low, a single course antibiotics might throw off the whole system. And then this tells you if pathogens are a potential issue driving your condition. So, then if it was a potential issue, then you would see the pathogens listed out here with what their levels are, the specific pathogens, and these are all the specific pathogens that are tested for. Is this scrolling up Michael? You can see this?
Michael Roesslein:
Yes.
Kiran Krishnan:
Okay. And so if none of them are out of range, if your pathogen levels are all totally fine, then we won’t show you any specific information. We’ll just show you the list of all the things that are tested so that you and your health practitioner know what was actually tested for. But let’s assume that one of these were out of range. We would give you the specific pathogen, how far they are out of range out of the normal population, and then there would be lifestyle, diet, and supplement recommendations that help target that type of pathogen and maybe bring back balance into the ecosystem.
Kiran Krishnan:
Now the next big picture, we’re starting to look at phylum levels. So, every bacteria in your microbiome or in the world can be basically classified into different phyla. In the gut microbiome, there’s six major phyla of bacteria. These are the largest groupings of bacteria. And we know from 15 years of microbiome studies that proportions of these phyla are profound in terms of how they impact your outcomes, and so we look at some of these dysbiosis ratios, we call it, whether it starts with your Firmicutes/ Bacteroidetes ratio.
Kiran Krishnan:
In this case, this individual tends to have a much higher ratio for Firmicutes/ Bacteroidetes, which is interesting because a lot of the studies show that if you tend to have higher levels of Firmicutes over Bacteroidetes, then you tend to have metabolic dysfunctions. So, I don’t know who this individual is, but more than likely they might suffer from weight issues because this is a characteristic ratio for those suffering with metabolic disorders and weight issues and it could be driven primarily by a dysfunction in this Firmicutes/ Bacteroidetes ratio.
Kiran Krishnan:
Then over here you get all of the nutrition, lifestyle and supplement recommendations if this ratio was off on what to do about it. Again, everything we test is actionable within the report. We go through a couple other ratios that have a significant effect that can affect your outcomes. We explain what the ratios are and of course what the lifestyle and nutrition and supplement recommendations are. Then the next part is we’re going in deeper into the microbiome and we’re looking at specific functional groups within the microbiome that conduct functions that are important to health, are correlated with disease and also correlated with symptoms and other outcomes, right? So these are very important ones and these are the functional aspects of the tests that will really tell you about what your microbiome tends to do and tends not to do. These can be really important.
Kiran Krishnan:
For example, we test groupings of ammonia producing bacteria and what is their relative abundance compared to other microbes within the microbiome. And this is really important because in this case, this person has really low levels of ammonia producing bacteria, which is good because if you tend to have higher levels of ammonia producing bacteria, what that means is, for example, a high protein diet wouldn’t be a good choice for you. A lot of people’s assume that a high protein diet is a good thing. Well, if you have high ammonia producing bacteria, what’s going to happen is you’re going to convert a lot more of that protein into ammonia, which will then become toxic to the liver. It’ll put stress on the liver and increase fatty acid production in the liver. It’ll increase the PH in the gut, which makes you more susceptible to fungal overgrowth and pathogen overgrowth as well.
Kiran Krishnan:
And then it also creates inflammation in the gut, right? So without knowing whether you have high ammonia producing bacteria, you may assume a higher protein diet is a good thing for you. But it’s actually not, and actually it could be the thing that’s actually keeping you from healing. You could be somebody that ate the standard American diet and now you’re going, “I’m cleaning up my diet because I want to improve my health. I’m going Lots of lean protein, some fermentable carbohydrates, some healthy fats. And that’s my diet.” Lots of Americans diet that way and presume it’s healthy for them, but you may not be getting better, and the reason may be because you have high ammonia producing bacteria that are converting that amino acid into ammonia. At the same time we look at the amount of ammonia clearing bacteria. This individual, they’re not producing much ammonia so they clearly don’t have higher levels of bacteria to clear the ammonia as well.
Kiran Krishnan:
So, this person is doing quite well. They can probably sustain a higher protein diet. Other types of functionalities to give you an example that we look at is sulfate-reducing bacteria. This individual tends to have very low levels of sulfate-reducing bacteria, which is a fine thing. You don’t want to have too low levels. You do need some sulfate reduction and we talk about that. What if sulfate reducing is low, what if sulfate reducing is high. We give you recommendations on that, but to give you an example of why this is important to understanding the function and dysfunction within your microbiome, there are lots of really healthy foods that tend to be high in sulfates. So foods like, apricots and cheeses like Parmesan cheese, seafood like red meat, eggs, onions, leeks, garlic, cabbage, brussels sprouts, all of these are perfectly healthy foods, but they tend to be high in sulfate.
Kiran Krishnan:
So when you have high sulfate-reducing bacteria, what’s going on is when you eat those foods, the high sulfate reducing bacteria are converting the sulfate in those foods into hydrogen sulfide and hydrogen sulfide is extremely inflammatory and toxic to the bowel, to the gut lining. And in fact, high levels of hydrogen sulfide are correlated with inflammatory bowel disease, right? So, you might think you are having an healthy diet, “Hey, I just ate a bunch of cabbage and Brussels sprouts and lean and healthy fish and an egg and some apricots on the side.” Well, that is typically a healthy diet for a lot of people, but because you have high sulfate-reducing bacteria that’s actually driving inflammation in your gut, you would never know that unless you had this kind of functional analysis within your microbiome. So, that’s why we think this type of functional analysis is so important versus just giving you a list of bacteria and telling you if they’re high or low, and each individual bacteria strain within your microbiome.
Kiran Krishnan:
Because it’s not telling you anything about the function of your microbiome. An individual that has high sulfate-reducing bacteria, maybe eating a seemingly perfectly healthy diet, but getting a lot of not healing or still getting a lot of symptoms and that’s because the bok choy and broccoli and asparagus and things like that that they’re eating are being converted into hydrogen sulfide. Right? So these are the functionalities we looked at methanogens, methane production. We look at estrobolome and a number of different functionalities including the dysbiosis ratio, the 31 in all functionalities. If you do the test tomorrow, the first report you get will have I think 19 of the 31 functionalities, but the moment the other functionalities are done, which we’re doing all of the genetic mapping and all that for that which we predict will be done in the next three four weeks, you’ll get an updated version of your report at no additional cost to look at the other functionalities as well.
Kiran Krishnan:
For example, one of the functionalities we’re looking at is, bacteria that produced your urolithin A. Right, and I’ve talked about your urolithin and the importance of that. Urolithin is for something that maintains healthy mitochondria that increases mitophagy, so the recycling of damaged mitochondria, it actually is one of the most powerful antioxidants in the gut and one of the most powerful antioxidants in mitochondria in your body. So it’s a super important compound and has all kinds of health implications and it has to be produced by converting polyphenols coming in from the diet into your urolithin. And there are groups of bacteria that do that and you wouldn’t know whether or not you need to increase your urolithin production in your gut by supporting those bacteria unless you had this type of functional analysis and low levels of your urolithin could be the biggest reason why you’re not healing or you’re not feeling enough energy being produced in your body.
Kiran Krishnan:
You’re feeling lethargic, you’re feeling tired, even though you’ve made all of these strides in your health journey. It could be the whole your ut side of things or short chain fatty acid production. So, we look at all those kinds of functionalities in a much more detailed way. This is the only microbiome analysis that provides you that kind of information. You’ve all heard me talk about Keystone strains in the next part of the test we, we look at all of the well established Keystone strains that are really important for the health of your microbiome for maintaining the ecological structure of your microbiome. And many of these Keystone trains have direct correlation to chronic illness and so we look at levels of your Keystone strains and map it against a healthy population. And of course if any of these Keystone strains are low, you get recommendations on how to increase them through diet, lifestyle and supplement modification as well.
Kiran Krishnan:
And that’s really important for the testing. And then finally you got an appendix. The appendix gives you different ways of visualizing all of the data that we talked about in the first part of the test. These are using doughnut plots and other charts that are color and metric. It’s not giving you any new information, it’s just a different way of visualizing the information and again, in my other videos I go through a much more detailed explanation of what to think about this aspect of the test. But here what we want to do is just give you a taste of the things that we look for in this new functional microbiome analysis. And keep in mind, we’re working with the absolute leader in this field, Dr. Rita Colwell. There is nobody else that comes even close to her pedigree in this particular field. And then the company that she’s built in CosmosID.
Kiran Krishnan:
So we’ve partnered with the absolute right people and we’re also using the whole genome sequencing, which is the new gold standard technology to detect bacteria at their species level. So, we’ve put together what we think is the most, functional, the stool tests with the most utility and one that’ll actually give you some guidance onto how to adjust your life for your diet and so on, to optimize your healing capacity in your gut. So that’s where the biome effects came in. So far we’ve just shipped out this week the first reports to the hundreds of people that have done the test. So we’re extremely excited to see what people’s responses are and see how this actually impacts how people figure out how to heal themselves or when you’re working with your health professional or doctor, how you guys work together to figure out what you need to do to heal yourself. So that’s the short version of the biome effects.
Michael Roesslein:
The short version, I had access to a sample report and I looked through it, but I didn’t understand it nearly as much as I do now. That’s pretty amazing and I have a lot of questions over here about how we’re going to work with this. We’re going to train a few coaches to give interpretations with this because yes, it has this report, but this is for practitioners. This is not intended to just be sent out and used by people without any training or any ability to interpret the test properly. It’s also not diagnostic. This is not going to diagnose anything or nothing like that.
Michael Roesslein:
So, we are going to train a few coaches in the next month and probably have this available sometime around mid March to our entire audience community. We will be able to order a test kit, take it at home, send it in and then when the report comes in we’ll have a coach that will go through your report with you. We should have that set up in less than a month. [inaudible 01:50:15] and I are going to work out the details of that and we’ll get that set up for you guys and it’ll be something that we’ll offer, so not today but sometime soon. We will be able to offer that. I have a few questions. I know we’re already going on two hours so, I’m going to try to keep them brief and if we need to I can email them to you.
Kiran Krishnan:
Yeah.
Michael Roesslein:
Can you ship this to New York?
Kiran Krishnan:
No. The city of New York will not allow us to ship it. The closest we can come is shipping it to New Jersey.
Michael Roesslein:
Yeah. That’s [inaudible 01:50:46].
Kiran Krishnan:
Yeah, which is what a lot of companies do, but when you take your sample, if the return address that you’re shipping it from is from New York, the lab can accept it. So you basically have to go to New Jersey and pick up kits or we can… We’re trying to figure out some sort of distribution system where we have kits available across the river in New Jersey and then a place to ship it back to lab from New Jersey as well.
Michael Roesslein:
Okay. Are you familiar with the test GutBiome+ from Psomagen?
Kiran Krishnan:
No, no.
Michael Roesslein:
Do probiotics need to be stopped?
Kiran Krishnan:
No. Absolutely not. I never understood-
Michael Roesslein:
Why [crosstalk 01:51:40].
Kiran Krishnan:
…that’s telling you that. Right? And my suspicion is because they’re afraid they’re going to pick up all the genetic elements from the probiotics. So people are taking all of these lactobacilli and that’s going to skew their reading of the tests. That again, is a problem if you’re doing 60 [nests 00:01:52:00] because you’re getting all of these fragments of all of your probiotics in there as well. But since we’re doing whole genome sequencing, it’s not an issue and we want to see what your micron looks like in reference to all the things you do. So stopping all the things you do, like probiotics and prebiotics and fermented foods and all that is meaningless because then your microbiome will revert or go back to a non-natural state for you. So we tell you don’t stop anything, even if you’re thinking into microbials, stay on them. Give us the sample now so we could tell you what it looks like based on everything you’re doing right now.
Michael Roesslein:
Okay. All right. There’s genetic information, personal data involved. A few people were concerned about how that’s being stored or shared or kept private.
Kiran Krishnan:
Yeah, so, if you look at this test, this is an actual person’s test, right? All of their genetic information and all that on the test is only identified by a sample ID, right? And then on a separate server, the ID is correlated to a person’s identity. So what it is, is all of the genetic information, all that is kept on one HIPAA regulated server and that’s really important to note. So, there’s all these HIPAA privacy medical laws and servers that contain medical information after we HIPAA complied. So they have to have all of these additional security systems and data transfer and all of that. So you’ve got all the genetic information that just stored as a sample ID that has no identifiable information on it. That’s why I have no idea whose tests this is. I just pulled one of the first batches of tests and then a separate server that contains the correlation to the actual individuals ID and then the program matches it and sends it to the person’s doctor.
Michael Roesslein:
Okay. Oh, I had a few questions about… Sorry, I was answering your question about last one and then we’ll go about Viome. My own personal response with Viome is that I’ve never been fully confident in it as a whole, as a company and this is mine, this is not your us. I don’t know your take on it, but the founder of Viome has some really shady skeezy business dealings in the past and very low integrity things that have happened in his business world and when that was brought to our attention, we were actually going to interview him for the human longevity project film series couple years ago.
Michael Roesslein:
And I think Jason actually did interview him and then we found out all that stuff and found out a whole bunch of other things and we pulled the content from the movie and personally, I’ve distanced myself in Rebel Health Tribe from Viome just because of that. And I didn’t feel that… I don’t know, there was something about it I didn’t trust. But what is the technology difference here? Is this different than that? And do you have an opinion on that test that you would be comfortable sharing?
Kiran Krishnan:
Yeah, so the Viome technology is a black box. They won’t talk about how they come up with the data. According to virtually every leading scientists in this field of metagenomics and all that, you cannot do what they do, right? And they get lambasted at scientific conferences. I’ve been to a number of scientific conferences where the chief science officer of Viome is sitting up there on a panel or does a presentation, and then the audience of researchers in this field are just hammering them because what they’re claiming that they’re doing, they’re taking RNA sequencing, not DNA. So they’re not doing DNA, they’re doing RNA sequencing and then they are making determinations of what type of metabolic processes are going on in the body based on that RNA sequencing and then making recommendations based on that.
Kiran Krishnan:
The problem is that technology doesn’t really exist. RNA is very unstable and they claim to be able to stabilize it for long periods of time, and I’ve sat next to researchers at conferences when they’re presenting and giggling at the data because when you look at the data, they show perfect lines and these perfect charts that really just don’t make sense in science and so it’s a Silicon Valley company.
Kiran Krishnan:
It’s funded by Silicon Valley type of money. I think there are notes, right? When you start thinking about Silicon Valley biotech type of things. So to me, it’s a really problematic thing. I wish they would be more upfront about their technology. I wish they would publish a paper, which would be great because if that technology does exist, then they shouldn’t be saying, “Oh, it’s secret. We can’t tell you how all of this is done. It’s in a black box and yet spinning out all these beautiful charts and all that, all the time.” Science is done by peer review and science has done by consortium and coming up with consensus among experts in the field. And so, when you have one company that claims that they have amazing space, age technology that nobody else who’s an expert in the field believes is possible, it becomes suspicious.
Kiran Krishnan:
So to me, I would never recommend anyone doing it. I’ve never done it myself. I’ve got a free box of it from one of the conferences I went to. I’ve never done it myself or sent it in. And it’s a completely different ballgame. They’re looking at RNA, not DNA. This is DNA sequencing. Also, the person whose scientific credentials that Viome is based on researcher that would, they initially use her name like I’m talking about Rita Colwell and all of her work. That person, Helen Messier left the company over a year ago. Right? So that’s never a good sign. Right? When the researcher and the decorated person that you’re basing the technology of your company around. If they leave for whatever reason, and that was quiet and high shots as to why she left one, when they leave that already signals issues.
Michael Roesslein:
Okay. Well that was very thorough. Mine was, I don’t like the guy. Kiran’s answer was much more founded in science. I think that’s good. If there’s any practitioners out there, they could sign up with an accounts with microbiome labs and they can access the tests. You’re making some training videos for the doctors practitioners. We’re going to use those to train our own coaches. The test is available now on there for professionals. We will have it available on our site soon for our audience to order and when your results come in, there will be a coach to go through the report with you. It’ll be optional if you want to do any further work with that coach. If you want to go down any other rabbit holes or any other testing or any other types of work with them, but they will be present to go through your report with you and help you make sense of it because that’s going to take some help and some practice.
Michael Roesslein:
It is super thorough and it is pretty straight forward, but I think it’s definitely responsible to have somebody who’s trained in the reports to go through it with people, to help them make a strategy going forward. So yeah, man. All right. I’m only 30 minutes behind schedule. I’ll walk 90 minutes this time instead of 60 because we always go over 60 and then I block 90 we go an hour or two hours. So, this is really impressive. I know how much work you guys have put into this behind the scenes. I know how long I suspended play. I talked to Acacia last week and I know what she’s gone through with it and we’re putting-
Kiran Krishnan:
Amazing. Yeah.
Michael Roesslein:
…all this stuff together.
Kiran Krishnan:
Yeah. Her team, like the recommendations for example, right? None of this is frou-frou stuff. Every recommendation that’s here has a scientific study that backs up the efficacy that we’re talking about and Acacia and our team have put together all of the reference lists. Now we don’t put the references on the report because this would literally be like a 75-page report. Right? And it would make people’s eyes glaze over. But we have all of these references, right? If somebody says, “Hey, where is your filters for this dysbiosis ratio for your recommendation here on the nutrition side?” We can provide those. Right? And the mapping work that has gone in it, it’s really an immense amount of work. I started having thought experiments about what I would want a microbiome test to look like in terms of what we test, what information we give people.
Kiran Krishnan:
This was a couple of years ago as I started getting pressure from people going, “Hey, you have microbiome labs, why don’t you come up with a better test? Don’t just tell us that other tests aren’t good enough. Come up with a better one.” And so I was like, “Oh, I guess they’re right to some degree.” And I started in my 16-hour flights. I sit in and I imagine all of these things and how to connect some of these things. This is a task I imagine, and we have an amazing team between CosmosID and our own team, that man, the amount of work they did to put this together, it’s really amazing. And I think it’s going to give a lot of people some really interesting clues as to what’s going on in that gut of theirs.
Michael Roesslein:
Sorry, I just got on me. Somebody knocked on our door. So the dogs haven’t. So I did a quick mute and then I started talking and I was gone. All right. Awesome. That is amazing. This is really cool. So, I’m excited about this. We’ve had a lot of questions. We will have it up in a few weeks and I will do another video then or we’ll do some sort of announcement. You’ll definitely know. For right now we have the Mega Omega and the Fido score in the shop, the code five Omega10. One word. It’s good for the weekend, 10% off of that. And yeah, man, thanks. It’s so crazy. when we first started working together, I think the office was like you had Tom and maybe three other people and now you have departments and-
Kiran Krishnan:
we have committees and we have 70 plus employees. We have an HR department. It’s absolutely insane and most excited about all of this is we have the resources to invest in research in a major way. You know, like what we’re doing with SAC state, the big studies we’re doing, with cancer and all that. I mean, that’s super exciting for us. Then that’s ultimately where we’re, where we get our biggest thrills and all of this.
Michael Roesslein:
Awesome. Well, thank you for doing all that. We’ll definitely do a field trip over to the lab and do some video over there and film over there. So, thanks everyone for attending. We had like no dropoff basically in two hours, which was insane. And we will get this recording transcribed and sent out probably Friday, maybe Saturday. So keep an eye out on your inbox for that.
Kiran Krishnan:
Yeah, thank you guys. Always a pleasure with the RHT. Thank you.
Michael Roesslein:
Take it easy, man. Good to see.
Kiran Krishnan:
You too. Bye-bye.
Gut Microbiome & Digestion Products
-
-
-
-
$119.98
ZenBiome™ Sleep is formulated to help clients deal with occasional...
Get Social
Recent Podcasts
Recent Courses
Toxicity & Detoxification Masterclass
The toxicity and Detoxification Masterclass covers a wide
5-Week Functional Neurology w/ Dr. Jared Seigler
Learn how to improve your brain health and
Brain & Nervous System Masterclass
16 Leading Experts Share Cutting-Edge Science, Effective Practices,
Wellness Optimization Series
Learn about the immune system and what you
Get the RHT Newsletter
Be the first to get access to special offers, new podcasts, courses, products and events from Rebel Health Tribe.
Facebook
Twitter
Pinterest
LinkedIn
Reddit
WhatsApp
Telegram
StumbleUpon
-
MegaSporeBiotic
$59.99 – $176.95MegaSporeBiotic™ is a 100% spore-based, broad-spectrum probiotic shown...
-
MegaSporeBiotic For Kids Gummies
$39.00MegaSporeBiotic™ Gummies are a 100% spore-based proprietary probiotic...
-
MegaMucosa
$59.99MegaMucosa is the first complete mucosal support supplement...
-
MegaPre Prebiotics Powder
$59.99MegaPreBiotic™ is the first Precision Prebiotic™ supplement made...

Meet Your Microbiome: The Human Microbiome and How to Optimize It
Meet Your Microbiome: The Human Microbiome and How to Optimize It On and in the average human, there reside approximately

Benefits of Probiotics Including Improved Gut Health
Benefits of Probiotics Including Improved Gut Health “Probiotics” has become quite the buzzword – with countless products and supplements proudly
Gut Microbiome Health and the Gut-Immune System Connection: Part 2 Lower GI
Gut Microbiome Health and the Gut-Immune System Connection: Part 2 Lower GI The diverse community of microbes in your digestive
Gut Microbiome Health and the Gut-Immune System Connection: Part 1 Upper GI
Gut Microbiome Health and the Gut-Immune System Connection: Part 1 Upper GI The message is out: gut health is critical