More Posts from
AutoImmune & Chronic Disease
Genetics and Hormone Production, Transport, Utilization, and Metabolism
Our genetics play a larger role in our hormones than
Genetics & Neurotransmitters: Impact on Your Mood, Energy, Hormones, and More!
Have you wondered why an antidepressant didn’t work for you?
Genetics and Detoxification: Your genes are key to knowing what detox protocol will best suit your body.
https://vimeo.com/821487331 If you’ve ever bought a detox kit off
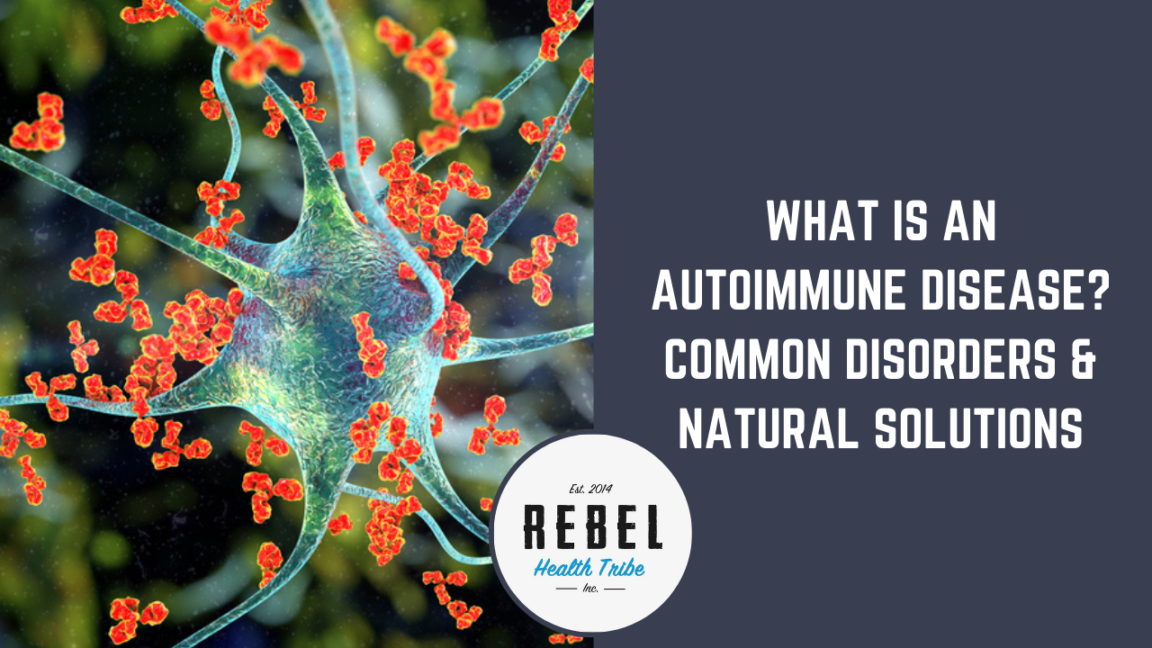
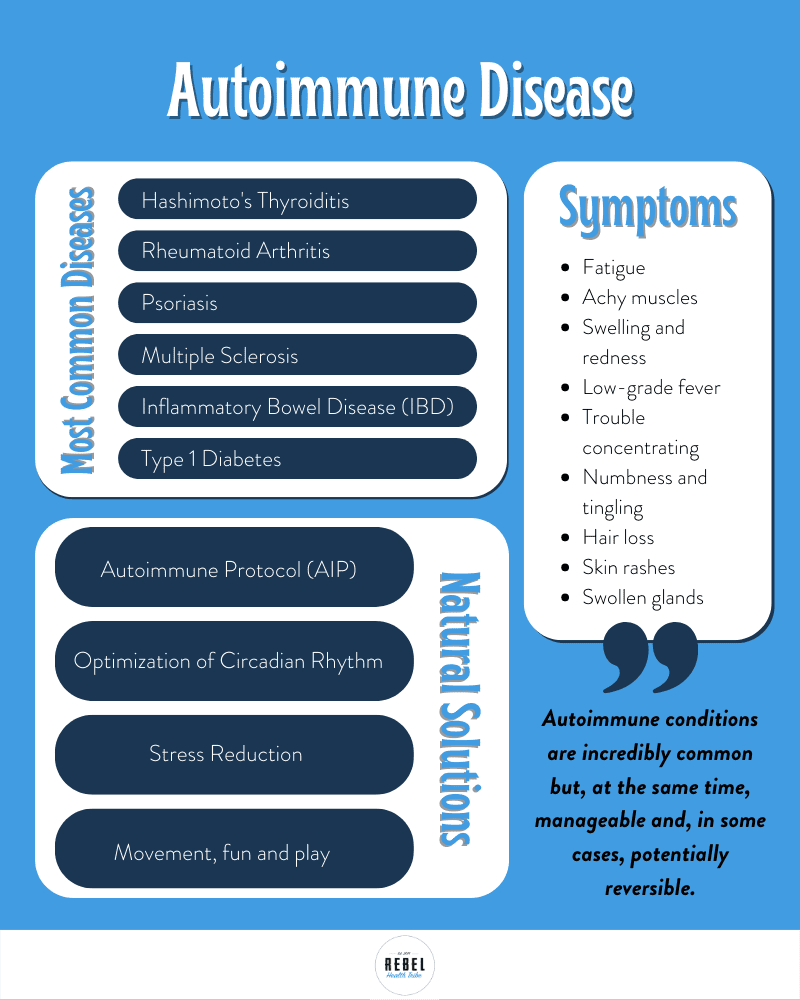
What is an Autoimmune Disease? Common Disorders & Natural Solutions
One of the most incredible aspects of the human body is its inborn ability to protect itself from the outside world. The body’s largest organ, the skin, is a literal physical barrier separating what makes you, you, from everything else.
Internally the body contains a complex network of processes that make up your immune system. When your physical barriers fail, the internal mechanisms get right to work to protect you from harm.
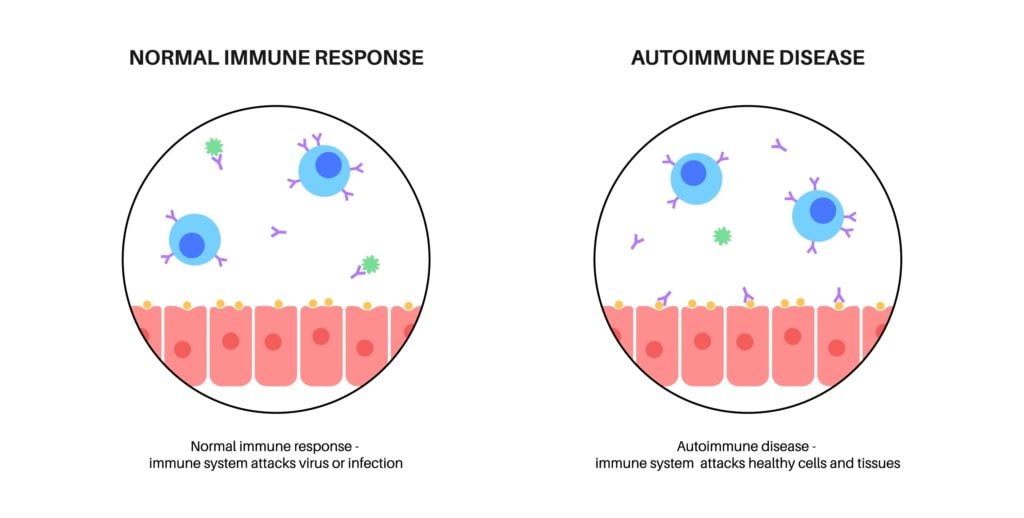
Unfortunately, like everything else, your immune system has the potential to go awry. Autoimmunity occurs when your immune system mistakenly attacks your own tissues. The consequences can be devastating.
More than 24 million people in the US suffer from an autoimmune condition, and the numbers are rising. Worldwide, upwards of 19% of the population has an autoimmune disease, up from 3.2% before 1995. Women make up at least 80% of autoimmune disorder patients.
What has led to this shocking rise in autoimmunity? And most importantly, how can we address it to repair our own and our family’s health?
In this article, we’ll take a closer look at the immune system and autoimmunity, including:
- How your immune system works under normal conditions
- The difference between innate and adaptive immunity
- The likely culprits of autoimmune disease
- A brief look at some of the most common autoimmune conditions
- Autoimmune symptoms and what to watch for
- Natural ways to address autoimmune issues
Immune System 101
The process by which your immune system responds to threats is truly fascinating. Sophisticated mechanisms are in place to identify a foreign pathogen that could make you sick.
When something foreign enters the body, the cells of your immune system get to work in a matter of seconds. A rapid cascade of events takes place to mount a response to neutralize the threat.
There are two basic phases to any immune response. One that happens almost instantaneously called the innate immune response, and the second that gradually ramps up called the adaptive immune response.
Let’s look at each of these in-depth.
“Autoimmunity occurs when your immune system mistakenly attacks your own tissues. The consequences can be devastating.”
Innate Immune System
The innate immune system is made up of the immunity you are naturally born with. When presented with a threat, your innate immune system responds immediately, in the same way, every time. It’s non-specific in that it cannot change how it responds depending on the challenge presented.
The innate immune system is made up of many different pieces. Some of them are barriers that prevent viruses and bacteria from entering the body. These include:
- The skin – Your first and most tangible protection from any outside element, the skin provides an obvious physical barrier to invasion. In addition, the skin’s pH creates an inhospitable environment for the growth of bacteria and other microorganisms. In case of a wound or injury, immune cells in the skin act to protect and repair the tissue.
- Mucous membranes – The digestive tract and airway are among the organ systems that use a mucous membrane as both a physical and chemical barrier. A good example is the mucous membrane inside your nose that traps and neutralizes dust and microbes.
- Stomach acid – The low pH of gastric juices naturally kills microorganisms ingested with food or drink.
If an invader makes it past one of the many physical barriers, immune cells spring into action. Again, these cells respond in programmed ways that are not specific to the invading virus or bacteria.
- Mast cells – these cells release a flood of cytokines that promote inflammation and rally other cells to attack the invader.
- Natural killer cells – these cells specialize in identifying aberrant cells or those that are not a normal part of the body. Once identified, they release toxins that neutralize them.
- Neutrophils – these cells engulf and destroy invading pathogens.
- Dendritic cells – these cells provide information to the adaptive immune system to stimulate a more specific immune response.
A key feature of the innate immune response is inflammation. Inflammation is critical to innate immunity and helps contain pathogens and alert other immune cells of danger. While an initial inflammatory response is necessary, problems arise if signals get crossed in the body, and the inflammation is never “turned off.” More on that later.
If an invader evades the innate immune system, the adaptive immune system jumps into action.
Adaptive Immune System
The body’s adaptive immune response takes time to ramp up. It is specific to the foreign invader, meaning the body has to develop the necessary cells to target the unique make-up of the virus or bacteria. It may be up to 96 hours before the adaptive immune system creates and releases antibodies.
Two types of immune cells are central to adaptive immunity.
- B cells – these cells produce antibodies that bind to pathogens and neutralize them.
- T cells – these cells target and destroy body cells that have been infected by a pathogen.
As the adaptive immune system takes over, anti-inflammatory signals calm the initial inflammation initiated by the innate immune response. This is critically important as prolonged inflammation can quickly move from helpful to harmful.
Unlike innate immunity, adaptive immunity has a memory. If your body has battled a pathogen before, the adaptive immune system remembers it and is likely to mount a faster and more effective response upon subsequent exposure.
While the innate and adaptive immune systems function differently, each relies on information and signals from the other. One of the most critical pieces of information both phases of the immune response require is the ability to differentiate self from non-self. Here is where things can get tricky.
Physiology of Autoimmunity
The immune system has a powerful ability to seek out and destroy cells it has identified as non-self, or essentially, invaders. Due to its potent killing power, the body maintains a system of protections meant to differentiate between self and non-self.
When these protections become imbalanced, immune cells get confused, and body cells that should be labeled “self” are identified as invaders. The result is an immune response targeting essential body tissues.
At its most basic, autoimmunity can be described as a “failure of self-tolerance.” Both the innate and adaptive immune responses suffer from dysregulation of the mechanisms that prevent targeting of self-tissues.
The adaptive immune response is often considered the primary culprit in autoimmunity. When the adaptive system becomes confused, it produces B and T cells meant to attack healthy tissues.
When the adaptive immune response is active, the innate immune system continues to chronically promote inflammation and immune cell activity that, over time, damages organs.
In contrast to a true foreign invader, your own body tissues are not going anywhere. This means that once an autoimmune reaction gets going, putting on the brakes is a challenge.
Identifying the root cause of autoimmune diseases is critical to effective treatment.
What Causes Autoimmune Disease?
Pinpointing the exact cause of someone’s autoimmune condition is a bit like determining which ingredient in a recipe is responsible for the final flavor. Many factors work together to create the conditions ripe for autoimmunity.
While there may not be just one answer to the root cause of autoimmune reactions, there are many clear players. Biggest among them is your genetics. Some people are born genetically predisposed to autoimmune disease.
However, just because someone has genes coded for autoimmunity doesn’t mean they will develop an autoimmune condition. Your genes are only one piece of the puzzle. Your environment is the main signaler telling your genes to express their code or not.
Many aspects of your environment influence your risk for an autoimmune condition. Here are just a few:
- Altered Microbiome – The diverse community of microbes(Link to microbiome article) in the gut is integral to the immune system. The microbiome is part of the gut mucosa, forming a physical barrier to protect against pathogens. In addition, the microbiome plays a regulatory role in balancing B and T cells as well as other important immune substrates. Dysbiosis of the microbiome is strongly associated with autoimmune conditions. When the essential work of the microbiome is disrupted, the immune system no longer functions smoothly, and the risk of a confused autoimmune response increases.
- Molecular Mimicry – The immune system can become confused when a pathogen such as a virus has a similar antigen structure to healthy body tissues. When this occurs, the immune system may become sensitized to body cells and inflict ongoing damage. To learn more about molecular mimicry, Dr. Kharrazian’s autoimmune Master Class is a great resource.
- Environmental Toxins – The list of problematic toxins in our everyday environment is much too long. Pesticides, silica, mercury, and cigarette smoke are just a few examples of toxins that trigger inflammation and potential autoimmunity.
- Systemic Inflammation – Systemic inflammation may occur if the innate immune system doesn’t receive the proper signals to turn off the inflammatory response. While inflammation is essential for the early stages of fighting an infection, over time, inflammation causes damage to normal tissues and keeps the immune system on constant alert, targeted at self-tissues.
- Stress or Trauma – While you may not think of stress or trauma as environmental triggers, they strain the body and compromise healthy immune function. In fact, the effects of stress and trauma are so far-reaching that the impact may be felt years or even decades later. One large-scale study found that the more stressful or traumatic events a child experienced, the more likely they would develop an autoimmune condition as an adult.
- Infection – A previous infection with a bacteria or virus can be a trigger for autoimmunity. While, of course, many people recover from infections with no lingering issues, for genetically susceptible individuals, their immune system is prone to get confused, raising the risk of an autoimmune condition. Exposure to the byproducts of cell destruction caused by the immune system’s response to an infection is one mechanism by which immune cells become reactive to body tissues. Another possible mechanism occurs if a virus damages the thymus, the site of T-cell screening and management. Disruption of normal thymus function may lead to dysfunctional T-cells entering the bloodstream when they would normally have been screened out.
Most Common Autoimmune Diseases
An autoimmune response can affect any body system, and the resulting damage disrupts normal organ and tissue function. Over 100 autoimmune conditions have been identified, but let’s take a brief look at a few of the most common autoimmune diseases.
Hashimoto’s Thyroiditis
The thyroid gland secretes essential hormones that regulate a range of body functions, including metabolism, temperature regulation, and healthy brain function. If the immune system attacks and damages the thyroid, eventually, the gland will no longer secrete adequate amounts of thyroid hormones.
Individuals with Hashimoto’s thyroiditis may experience fatigue, weight gain, loss of cold tolerance, muscle aches and weakness, and depression.
Rheumatoid Arthritis (RA)
RA occurs when the immune system attacks the joints of the body, causing inflammation and swelling of the joint tissues. Without proper treatment, RA leads to irreversible damage to the lining of the joints causing chronic pain and malformations.
Psoriasis
When the immune system attacks skin cells, it may cause them to multiply rapidly. This leads to raised, scaly patches of skin that often burn or itch. Psoriasis can also impact the organs, and a third of people with the autoimmune condition also develop psoriatic arthritis, causing swelling, pain, and damage to the joints.
Psoriasis is one type of autoimmune disease that flares up and then temporarily subsides. Individuals with psoriasis are often able to link certain triggers to a flare-up. Identifying habits that trigger an autoimmune flare opens the possibility of interrupting the process and signaling the immune system to calm down—more on that in a bit.
Multiple Sclerosis
Multiple sclerosis (MS) is an autoimmune disease in which the immune system attacks the protective sheath called myelin that surrounds nerve tissues. Damage to myelin disrupts normal communication between nerves, interfering with the brain’s ability to send nerve signals to the body. Over time, nerve damage accumulates, leading to an array of neurological symptoms such as gait problems, numbness and weakness in the limbs, fatigue, and vision issues.
MS is another autoimmune condition that goes in cycles of flare-ups followed by remission. It is a relapsing-remitting disease for a majority of people. Some people may go years between relapses.
Inflammatory Bowel Disease
Inflammatory bowel disease (IBD) occurs when the immune system attacks the gastrointestinal tract. As a result of the autoimmune response, the lining of the intestines becomes inflamed and damaged, leading to not only gastrointestinal symptoms such as constipation, diarrhea, gas, bloating, and food intolerances but also weight loss and fatigue.
In addition, individuals with IBD are significantly more likely to also suffer from other autoimmune conditions. Because the digestive tract and microbiome play such an important role in immune regulation, it makes sense that an autoimmune condition that damages the gut would increase the risk of additional autoimmune issues.
Type 1 Diabetes
Type 1 diabetes occurs when the immune system attacks cells in the pancreas that produce insulin. The autoimmune disease is known as an “organ-specific” autoimmune condition as it narrowly targets the beta cells of the pancreas. While type 1 diabetes is often diagnosed in childhood, the condition can affect people of any age.
Interestingly, individuals with type 1 diabetes are at high risk of developing other organ-specific autoimmune conditions. The most common is thyroiditis.
Autoimmune Disease Symptoms
Determining whether you have an autoimmune disease requires a close look at your symptoms. A skilled healthcare practitioner will also delve deep into your family history, health history, as well as any relevant testing.
While symptoms will vary depending on the organ system being affected, many autoimmune disorders share similar signs in the early stages. Consider reaching out to your healthcare provider if you are concerned about some of these common symptoms of an autoimmune condition:
- Fatigue
- Achy muscles
- Swelling and redness
- Low-grade fever
- Trouble concentrating
- Numbness and tingling in the hands and feet
- Hair loss
- Skin rashes
- Swollen glands
As the condition progresses, symptoms may become more specific to the body tissues and organs affected. For example, in RA, the joints become inflamed and swollen.
“In addition to the treatment available through conventional medicine, many natural solutions can help manage symptoms. There have even been reports of natural remedies for autoimmune disease reversing the course of illness for some people.”
Natural Solutions for Autoimmune Disease
As autoimmune conditions have become increasingly common, our understanding of treatment options has expanded. In addition to the treatment available through conventional medicine, many natural solutions can help manage symptoms. There have even been reports of natural remedies for autoimmune disease reversing the course of illness for some people. One example is Dr. Terry Wahls, who has an amazing story of using natural techniques to halt the progression of her MS.
Whatever your goal for your autoimmune disease, natural remedies are good for your overall health and aid in regulating your immune system. Some people report improvement in symptoms and longer time between flare-ups when they focus on healthy, natural lifestyle habits.
Here are a few natural remedies that may be beneficial:
Autoimmune protocol (AIP) – The autoimmune protocol diet aims to heal the gut and microbiome, repair leaky gut, and decrease systemic inflammation. It works in two phases, starting with elimination, where the individual removes all foods that have the potential to negatively affect the gut, such as grains, legumes, nightshade vegetables, and sugar. Once someone experiences relief from autoimmune symptoms, they can move on to phase 2, where they may slowly reintroduce foods one at a time, watching to see if any food triggers a flare-up.
At all times, AIP encourages a healthy, nutrient-dense diet made up of whole, minimally processed food.
Studies of the AIP diet show promising results in improving symptoms, reducing inflammatory markers in the body, and increasing quality of life.
Optimize circadian rhythm/sleep cycles – Nothing functions well in the body without adequate, restful sleep. The immune system is no exception.
Poor sleep is associated with an increased risk of autoimmune disorders. One interesting mouse study demonstrated the earlier onset of autoimmune disease in mice who experienced sleep deprivation vs. those who did not. Sleep is truly foundational to health, well-being, and a strong immune system.
Engaging in good sleep habits such as establishing regular sleep and wake times, having a soothing bedtime routine, optimizing light exposure, and limiting sleep disruptors near bedtime, play an important role in getting a good night’s rest every night.
Stress reduction – Chronic stress activates the sympathetic nervous system, keeping the body in fight or flight mode. When the sympathetic nervous system is chronically active, immune function is impaired, and systemic inflammation is triggered. Part of this effect is caused by elevated levels of the neuroendocrine hormones released during stress. These hormones disrupt normal immune function, laying the groundwork for autoimmunity.
Reducing stress should be a pillar of treatment for autoimmune conditions. Activities such as exercise, social connection, meditation, yoga, and time in nature promote activation of the parasympathetic nervous system, calming stress.
Movement, play, and fun – Human bodies are made for movement and play. Whether structured exercise, sports, walking, or active social games, physical activity can be a key part of effective autoimmune disease treatment.
Physical activity stimulates the growth of cells that regulate immune cells. For anyone with an autoimmune condition, boosting the body’s ability to self-regulate immunity is essential! Exercise is a natural way to do just that.
In addition, being active naturally reduces systemic inflammation. Physical activity is so important for healthy immune function that studies show lack of physical activity is a risk factor for autoimmunity. Thankfully, increasing your movement can help.
Please note that this is NOT medical advice. Autoimmune diseases can be very serious, and you should be working with a professional. There are also times when conventional medications are essential for reducing/managing symptoms while exploring a more holistic approach.
Take Away
Autoimmune conditions are incredibly common but, at the same time, manageable and, in some cases, potentially reversible. If you are one of the many people suffering symptoms of an autoimmune disease, seek help and start on the path to repairing and regulating your immune system.
For more detailed information, check out our Autoimmune Masterclass. We brought together 21 of the world’s leading doctors, researchers, and experts on autoimmunity to teach you all you need to know to prevent autoimmune disease from impacting your long-term health and well-being.
RHT Gut Repair & Microbiome Optimization Guide
10 Steps to Repair Your Gut, Optimize Your Digestion, and Build a Healthy Microbiome!
- The top recommendations from 50+ hours of gut & microbiome webinars
- Easy-to-digest (get it?!), simple, and practical suggestions you can start right away
- What to eat for a happy, healthy, and diverse microbiome
- “Disease begins in the gut” - and so does health! Let’s turn it around!

FEATURED PRODUCTS
-
MegaSporeBiotic
$59.99 – $176.95MegaSporeBiotic™ is a 100% spore-based, broad-spectrum probiotic shown to be...
-
MegaSporeBiotic For Kids Gummies
$39.00MegaSporeBiotic™ Gummies are a 100% spore-based proprietary probiotic blend that...
-
MegaMucosa
$59.99MegaMucosa is the first complete mucosal support supplement of its...
-
MegaPre Prebiotics Powder
$59.99MegaPreBiotic™ is the first Precision Prebiotic™ supplement made up of...
Get Social
Recent Podcasts
Recent Courses
Toxicity & Detoxification Masterclass
The toxicity and Detoxification Masterclass covers a wide
5-Week Functional Neurology w/ Dr. Jared Seigler
Learn how to improve your brain health and
Brain & Nervous System Masterclass
16 Leading Experts Share Cutting-Edge Science, Effective Practices,
Wellness Optimization Series
Learn about the immune system and what you
Get the RHT Newsletter
Be the first to get access to special offers, new podcasts, courses, products and events from Rebel Health Tribe.
Facebook
Twitter
Pinterest
LinkedIn
Reddit
WhatsApp
Telegram
StumbleUpon
-
MegaSporeBiotic
$59.99 – $176.95MegaSporeBiotic™ is a 100% spore-based, broad-spectrum probiotic shown...
-
MegaSporeBiotic For Kids Gummies
$39.00MegaSporeBiotic™ Gummies are a 100% spore-based proprietary probiotic...
-
MegaMucosa
$59.99MegaMucosa is the first complete mucosal support supplement...
-
MegaPre Prebiotics Powder
$59.99MegaPreBiotic™ is the first Precision Prebiotic™ supplement made...
Toxicity & Detoxification Masterclass
The toxicity and Detoxification Masterclass covers a wide array of topics with the following guests: 1. Lara Adler, Environmental Toxins
5-Week Functional Neurology w/ Dr. Jared Seigler
Learn how to improve your brain health and function with this Functional Neurology course from Dr. Jared Seigler.
Dr. Seigler
Brain & Nervous System Masterclass
16 Leading Experts Share Cutting-Edge Science, Effective Practices, and Clinical Strategies to Optimize Brain & Nervous System Health in Kids