FAST DELIVERY
FREE SHIPPING OVER $150
90 DAY RETURN POLICY
HIGH QUALITY PRODUCTS ONLY
Description
The Supernatant Synbiotic Formula is an effective antimicrobial.* BioImmersion’s advanced Super Blend of naturally occurring whole probiotic organisms with their Supernatant metabolites and microRNA (ORNs – Oligoribonucleotides) contains important nutrients and factors that help protect and balance the gut microbiota. 34 billion CFU per gram.*
Supernatant (or as some call it postbiotic or parabiotic) is the fermented “soup” that contains powerful probiotic metabolites: enzymes, such as bile hydrolase, lactase, and others, peptides, proteins, vitamins, short chain fatty acids, bacteriocins, biosurfactants, microRNA or ORNs, and other nutritional substances. Supernatant and microRNAs are the power behind the new emerging research on immune-biotics: the antimicrobial qualities exerted by probiotics and their metabolites (Arena et al., 2018).*
Features / Benefits:
- Vegan
- NonGMO
- Kosher
- Free of Gluten
- Soy free
- Dairy free
- Protect and balance the gut microbiota
- Contains powerful probiotic metabolites
- One capsule a day for energy and endurance.
SUPERNATANT SYNBIOTIC FORMULA
BioImmersion’s Probiotic Super Blend is an advanced formulation of naturally occurring whole probiotic organisms with their Supernatant metabolites and Oligoribonucleotides (ORNs or MicroRNA). 30 billion CFU per gram.*
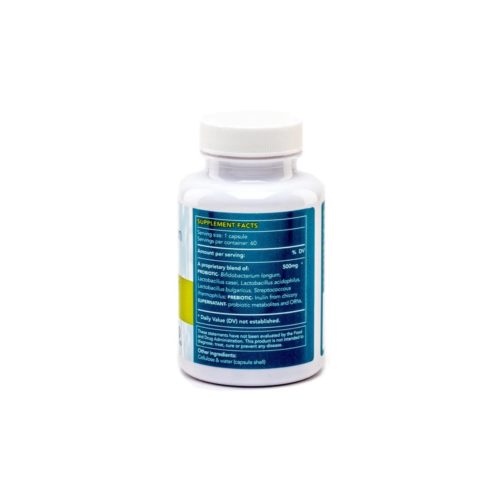
The super blend includes: Probiotics-Bifidobacterium longum, Lactobacillus casei, Lactobacillus acidophilus, Lactobacillus bulgaricus, Streptococcus thermophilus; Prebiotics- Inulin from Chicory root; Supernatant [or postbiotic]– a nutritional metabolites “soup” that is created from each of the probiotic organisms, which include their lactic acid, enzymes, vitamins, short-chain fatty acids, bacteriocins, bio-surfactants, bile salt hydrolase, and their ORNs (Oligoribonucleotides; microRNA). The supernatant is freeze-dried along with the good bacteria to form a powerful antimicrobial formula.*
Short chain fatty acids are also known to be the main nutritive energy source for the enterocytes (cells of the intestinal lining), hence, increasing production of short chain fatty acids improves the overall integrity of the GI tract membrane and tightening up cell junctions.*
Our probiotics are naturally occurring, whole organisms with their microRNAs (what ORNs are made of), they wake up quickly and are ready to multiply and build a robust healthy ecosystem in our alimentary canal, from mouth to anus. In order for probiotic to multiply, they need particular foods: dietary fiber and prebiotics they can metabolized in the GI Tract. Inulin, polyphenols, and beta glucan have been found to be excellent sources of fiber and prebiotic for microbes to ferment and metabolize (Holscher & Holscher et al., 2017; 2015, Etxeberria et al., 2013). The Supernatant Synbiotic formula is Vegan, Kosher, Non GMO, and free of Dairy, Soy, and Gluten.*
Supernatant Synbiotic Formula was developed to address the mounting problem of life-threatening hospital generated infections (nosocomal infections) from organisms such as C. difficele, Staph aureus, Klebseilla, and vancomycin-resistant Enterococcus faecium. The formula is comprised of supernatant’s many nutrients including the well-researched antibacterial substances such as bacteriocins, which suppress the growth of pathogenic bacteria (Cotter & Hill, 2013). Probiotics and their supernatant’s metabolites, including microRNA (or ORNs) are shown in research to regulate a balanced ecosystem in the GI tract and protect against bacterial pathogens (Aguilar et al., 2019; Chenoll et al., 2017; Goldenberg et al., 2013; Górska et al., 2016; Kawahara et al., 2015).*
A synbiotic: Synbiotic is defined as a “mixture of a prebiotic and a probiotic that beneficially affects the host by enhancing the survival and the implantation of live microbial dietary supplements in the gut, by selectively stimulating growth and/or activating the metabolism of a specific or few number of health-promoting bacteria” (Gibson & Roberfroid, 1995; Roberfroid, 2002). Most of BioImmersion’s probiotics formulas are synbiotics, which means they include prebiotics from plant fibers and inulin from chicory root. Inulin is naturally found in many different plant foods, such as garlic, onions, asparagus, chicory, artichokes, bananas, and more (Gibson et al., 1994; 2010).*
The Microbiome Project has taught us thathuman microbiota, the microorganisms that live inside us (GI Tract, mouth, vagina) and on us (skin), consist of trillion symbiotic microbes (Ursell et al., 2012). First coined as “microbiome” by Joshua Lederberg in 2001, microbiome is the combined genes of the microbiota, and signifies “the ecological community of commensal, symbiotic, and pathogenic microorganism that literally share our body space and have been all but ignored as determinants of health and disease.” In other words, the microbial communities. Rob Knight emphasizes that there are10 trillion human cells to 100 trillion microbial cells (2017, TED talk) – which means, there are more of ‘them’ than of ‘us.’ Aptly, Turnbaugh et al. (2012) describes this amazing genome collective of human and ‘other’ as a human “supra-organism.”
Supra-Organism: How do we achieve harmony and health as a human supra-organism? Just like plants rely on their microbiome for life-support functions (e.g., nutrients acquisition and protection against stressors and pathogens), so do humans rely on their microbiome for better health (Pérez-Jaramillo et al., 2018). Since each person embodies a unique system of human genes as well as harbors a “core set of specific bacterial taxa” (Qin et al., 2010), researchers are coming to the conclusion that plant-based foods healthily build our body cells and contribute the right nutrients and fiber to our core microbiota. In essence, researchers of traditional tribes find that the ‘hunter-gather’ still eats more plant-based diet, high in fiber, and very low animal meat, while the Western or modern societies eat protein and meat intensive diets (Caprara, 2018; Desmond et al., 2018; Gomez et al., 2016; Obregon-Tito et al., 2015; Schnorr et al., 2016, 2014; Turnbaugh et al., 2009; Ley et al., 2006).
Hence, achieving a healthy ‘supra-organism’ requires a combination of plant-based foods that nourishes and healthily feed both micro-organisms and human beings — precisely the principles that BioImmersion employ in the super blend and other formulations. To quickly form healthy colonies, organisms must have the type of foods they need – plant fiber and polyphenols. Food & microbial science show a special interactive relationship between polyphenols from plant-foods and probiotics–a ‘two-way relationship between polyphenols ←→ microbiotia,’ each helps the other, and together they modulate the gut microbiota to benefit human health (Cardona et al., 2013; Pathak et al., 2018).
MICROBIAL ECOLOGY
History: Probiotics are transient organisms found in a variety of fermented foods, from grains, to fruits, vegetables, legumes like soy, and dairy. Historically, these foods were consumed daily in every part of the world. Probiotic microorganisms belong mostly to the following genera: Lactobacillus, Bifidobacterium, and Lactococus, Streptococcus, Enterococcus (Markowiak & Śliżewska, 2017).
In 1965, Lilly & Stillwell defined the meaning of probiotics as substances produced by protozoan which stimulated another organism, in opposition to antibiotic which inhibits or kills other organisms. Parker (1974) later defined probiotics as ‘organisms and substances which contribute to intestinal microbial balance,’ while Savage (1977) described the microbial ecology of the gastrointestinal tract as “1014 [100 trillion] indigenous prokaryotic and eukaryotic microbial cells” (p. 107). Microbial organisms were further described by Fuller (1989; 1992) as a supplemental food, ‘live microbial feed supplement’ that effect the host (animal or human) by improving intestinal microbial ecology and balance. The World Health Organization (WHO) and the Food and Agriculture Organization (FAO) of the United Nations defined probiotics as “live microorganisms which when administered in adequate amount confer a health benefits on the host” (2001; see also Tufarelli & laudadio, 2016).
In October 2013, the International Scientific Association gathered an expert panel to redefine and discuss probiotics. The agreement that probiotics confer health benefits was reinforced, and a more accurate wording was used to describe probiotics as, “live microorganisms that, when administered in adequate amounts, confer a health benefit on the host” (Hill et al., 2014). In this way, the panel differentiated between probiotics as microorganisms and the commensals that are natural in the gut microbiota. However, when these commensal strains are collected from the gut, isolated, and characterized as giving health benefits, they can then be referred to as probiotics. In other words, probiotics need to show they are effective. Unfortunately, the term probiotic is used to sell skin care, shampoos and all sorts of other products, without the due diligence that signify the effectiveness of the probiotic, and therefore, misleading the public. To use the term ‘probiotic’ – a health effect must be shown (Hill et al., 2014).
Lactic acid bacterial (LAB): LAB species typically produce lactic acid as a main end-product of carbohydrate and fiber fermentation. LAB organisms are known for their adhesion to the mucus layer of the GI tract. This mucus layer plays an important role in protecting the intestinal epithelial cells against pathogens and damage, as well as provide a perfect milieu for LAB organisms to attach, grow and form their communities (Nishiyama et al., 2016). Streptococcus thermophilus is not part of the Lactobacillus species although this microorganism is also considered a lactic acid bacterium (Kechagia et al., 2012). Bifidobacterium uses a different metabolic pathway, and its name is actually a ‘misnomer’ as very few Bifidobacterium adopt a bifid morphology (even when exposed to stressful conditions), while the rod structure is the intrinsic morphology of the majority (Rajashekharan et al., 2017).
Beneficial Microbiota Milieu: Probiotic organisms have the potential to shift the gut microbiota milieu (composition) from a pathogenic predominance to a more beneficial micro-biotic ecosystem (Costello et al., 2012; Schnorr et al., 2016; Zitvogel et al., 2017). The fermentation process by probiotics in the gut microbiota keep at bay harmful pathogens by preventing their growth (Anzaku & Pedro, 2017). They assist the body’s immune system and contribute to a host of other positive health benefits. When the balance in the microbiome shifts toward a pathogenic community, it weakens the abilities of the helpful microbiota communities. An impaired microbiome is repeatedly shown in research to lead into conditions such as obesity, inflammatory bowel diseases, and other chronic illnesses (Patil et al., 2012; Schnorr et al., 2016; Kobyliak et al., 2016).
An important conversation in the scientific community is the role probiotic play in creating or modifying the composition of the gut microbiota toward better health (Sanders et al., 2018; Bron et al., 2017; Sanders, 2016). Globally, obesity is progressing and almost at the level of a pandemic, causing other chronic metabolic diseases to manifest (Dahiya et al., 2017). Since probiotics are transient in nature, and the gut lining continues to shed and renew its cells, how long do probiotic microbes stay in the gastrointestinal tract? And does a shorter duration have a power to create a healthy microbiome? Some say that although probiotics may not reside in the gut longer than two weeks, they do offer many benefits (Sanders et al., 2018), while others see a need for more specific research on fecal microbiota and probiotics (Kristensen et al., 2016).
At the core of this discussion is the need for a unified global regulatory frameworks and research methods, including a universal classification (nomenclature) of probiotic organisms to decrease consumer confusion and improve the scientific requirement for the commercial industry at large (Sanders et al., 2011). The gut microbial community includes bacteria (anaerobic and aerobic), viruses, fungi, with a variety of disease-causing pathogens and parasites (Howarth & Wang, 2013). Some microorganisms are shown to be helpful for human health, while others cause much distress. We have discussed how our diet, in particular, heavy consumption of meat, eggs, and dairy, change the composition of the microbiome (Matthews et al., 2018; Singh et al., 2017), but moreover, exposure to pesticides and herbicides (Stanaway et al., 2017), and other foods and environmental chemicals (Roca-Saavedra et al., 2017), create a heavy burden on the body’s ability to function well. As research continues to uncover new facets of research on micro-organisms, including probiotics, we will update this document. Stay tune also to Seann Bardell’s Forward Thinking emails found in the News within the Resources tab: http://blog.bioimmersion.com.
What do probiotic achieve in our GI Tract? Although the gut microbiome is a complex ecosystem of microorganisms, probiotics have exhibited many health benefits, including weight loss and improvement of metabolic diseases (Dahiya et al., 2017), boosting and supporting the immune system (de Vos et al., 2017), strengthening the intestinal barrier function (Blackwood et al., 2017), supporting colicky babies (Rhoads et al., 2018; Pärtty et al., 2012), and of course competing against pathogenic bacteria (Szajewska et al., 2016; Ayala et al., 2014; Johnston et al., 2012; Manzoni et al., 2006).
Even more so, probiotic organisms perform multitudes of other beneficial functions in the body: research shows that probiotics help to lower toxins (Yu et al., 2016; Qixiao et al., 2015; Amalaradjou & Bhunia, 2012), keep cholesterol down (Cani et al., 2011, 2009), assist in weight management (Everard & Cani, 2013), digestion and absorption of nutrients (Wang & Ji, 2018; Francavilla et al., 2017), elimination (Eskesen et al., 2015; Dimidi et al., 2014), and even function as anti-aging mediators (Buford, 2017; Nagpal et al., 2018). In other words, probiotics are shown in research to maintain a healthy ecological balance in the human gut and perform many beneficial functions.
SUPERNATAT
What is supernatant? Supernatant is the fermented medium created during the culturing process of probiotics. Supernatant is the fermented “soup” that contains important probiotic metabolites, such as enzymes, peptides, proteins, vitamins, short chain fatty acids, and other nutrients and factors, including antimicrobials such as Bacteriocins that may be used as a possible alternative to antibiotics (Cotter, Ross, & Hill, 2013; Yang et al., 2014). Supernatant, or as some call it, “postbiotic” (Auilar-Toalá et al., 2018), or “parabiotic” (Choudhury & Kamilya, 2018), is shown in research to have powerful antimicrobial properties with the potential to block adhesion, invasion and translocation of E. coli, yet it is gentle enough to be used to ‘enhance neonatal resistance to systemic Escherichia coli K1 infection by accelerating development of intestinal defense’ (He et al., 2017). In fact, Lazar et al.’s (2009) in vitro study concluded that the soluble probiotic metabolites, or supernatant, might actually interfere with the beginning stages of adherence and colonization of selected E. coli. This means that the supernatant itself exudes protective effects (Lazar et al., 2009), as well as work synergistically with probiotic organisms to stimulate the immune system against pathogenic invasion (Ditu et al., 2014).
Immunobiotics: The combination of lactic acid bacteria (LAB) and their metabolites is given much consideration as a method to improve human immune response against viral and fungal overgrowth. The term “immunobiotic” is a relatively new way to describe the antimicrobial qualities exerted by probiotics and their metabolites (Arena et al., 2018). The term ‘immunobiotic’ has been proposed to define beneficial microbes with the ability to regulate the immune system and lower inflammation of the gut tissue (Villena & Kitazawa, 2017; Villena et al., 2016). For example, the probiotics L. rhamnosus and L. plantarum carry immunobiotic properties and are shown to increase protection against viral intestinal infections (Albarracin et al., 2017). In a different study on mice, Kikuchi et al. (2014) discovered that oral administration of L. plantarum enhanced IgA secretion in both intestine and lung tissues, supporting against influenza virus infection. Immunobiotics, the combination of probiotics and their supernatant metabolites, have been found to support and benefit respiratory immunity (Zelaya et al., 2016), modulate mucosal cytokine profiles, IgA levels, and more, in various conditions of gastrointestinal inflammation (Carvalho et al., 2017).
Bacteriocins and Antimicrobial Properties: One of the properties that is given much attention is the bacterially produced antimicrobial peptides of bacteriocins (e.g., Cotter & Hill, 2013; Yang et al., 2014; Cotter et al., 2005). Already in 2005, Cotter & Hill observed that bacteriocin nisin functions by binding to lipid II, which is also the target of vancomycin antibiotic. This led to the suggestion that ‘bacteriocin nisin’ could be used as a template to design novel drugs. In 2018, the research to discover the mechanism of bacteriocin against pathogenic activity, including Staphylococcus aureus, continued with the discovery of critical features in the structure of bacteriocins that gives it such a ‘potent activity against pathogenic staphylococci’ (O’Connor et al., 2018).
Metabolic Disorders: Intestinal dysbiosis and endotoxemia have been linked to metabolic disorders: obesity, insulin resistance, and type 2 diabetes (Leite et al., 2017). Bacterial lipopolysaccharides (LPS) is a molecular element of the outer membrane of Gram-negative bacteria, and typically consist of lipid A (or endotoxin), a ‘core’ oligosaccharide, and a distal polysaccharide, (or O-antigen). LPS also are found in diverse Gram-negative bacteria, many of which are pathogenic to both humans and plants (Raetz & Whitfield, 2002). LPS (also termed endotoxin) serves as a shield from the environment and at the same time is recognized by the immune system as a marker for the entrance (or invasion) of pathogens, which in turn causes inflammatory response, and in an extreme response can bring about endotoxic shock (Rosenfeld & Shai, 2006). LPS causes inflammatory immunogens that circulate at low grade levels in healthy individuals, while high continuous levels instigate pro-inflammatory markers in the blood, e.g., interleukin-6, interleukin-1-alpha, interferon-gamma, triglycerides and post-prandial insulin. Proinflammatory markers are correlated with the risk of developing a variety of chronic illness, including increase risk of atherosclerosis (Erridge et al., 2007; see Cani et al., 2007).
Since the body is a mechanism of many interactive systems and components, a reaction in one system can instigate a positive or a negative chain of events in another. For example, in a clinical study, Leite et al. (2017) demonstrated that Gram-negative species (e.g., Bacteroides vulgatus and rodentium) were found in stools of individuals with type 2 diabetes, as well as an increase of pro-inflammatory interleukin-6 (IL-6) in their plasma. In other words, gut dysbiosis and metabolic endotoxemia have been linked to metabolic disorders, such as obesity, diabetes, and insulin resistance (van Olden et al., 2015). The gut microbiota contributes to many processes in the human host’s body, and the host provides a place of residence for the survival of the microorganisms (Leite et al., 2017). This give and take relationship has to be delicately balanced.
Epigenetic Changes: Bhat et al. (2017) considers dietary metabolites that are derived from the gut microbiotic population as critical modulators of epigenetic changes in both animals and humans. Nutrients in the gut are produced by microbial metabolisms of fiber, which means that short-chain fatty acids, polyamines, polyphenols, vitamins, and other metabolites, participate in “various epigenomic mechanisms that reprogram the genome by altering the transcriptional machinery of a cell in response to environmental stimuli” (Bhat et al., 2017). In other words, what we eat does modulate our gut which in turn can influence our health through modulations of genes.
Potent Immune Boosting Nutrients: Adding the natural supernatant metabolic ‘soup’ of potent nutrients that probiotic organisms create while they grow and multiply is showing great potential for human health. Immunobiotics is a study field that endeavors to understand how microorganisms and their supernatant interact with the immune system to support a healthy functioning body (e.g., Górska et al., 2016). Studies on probiotics and their supernatant metabolites are ongoing and add much to our understanding of Turnbaugh et al. (2012) “supra-organism” description of our bodies as an amazing genome collective of human cells and ‘other’ cells.
Continue to learn what supernatant and probiotics do by reading articles in the Research tab.
microRNA or ORNs (Oligoribonucleotides)
History: Probiotics have had a long history in helping farmed animals combat gut disfunctions caused by overuse of antibiotics to stimulate faster growth. In the 1950s the readily available antibiotics gave rise to the concern that using it as a substance to promote growth was creating resistant populations of bacteria, which means that antibiotics would lose effectiveness against infections from bacteria. Although in 1969 antibiotics were restricted as a growth promotor, the use has not subsided until very recently with the rise of organic and grass-fed animal farms. Fuller (1989) noted that antibiotics have a long-lasting upsetting effect in the gut because of the imbalance caused in the indigenous gut flora. In today’s language, antibiotics disrupt the natural microbiome, causing various diseases (Langdon et al., 2016). Probiotics offer a practical solution as an alternative therapy. For example, they exert antimicrobial properties by inhibiting adhesion of pathogens to the mucosa (Salas-Jara et al., 2016; Chenoll et al., 2011), or produce bacteriocins lethal to the pathogens, as we have seen above in the supernatant section (Reid & Burton, 2002)
MicroRNA Immune-Modulating: Bacteria release immune-modulating molecules when entering the mouth, such as ribonucleic acid or RNA, as though they are ready to defend themselves. Small pieces of RNA, called MicroRNA (miRNA) or oligoribonucleotides (ORNs), are released by pathogenic bacteria as well as a beneficial bacterium such as Lactobacillus casei, which we find in fermented foods like yogurts. Other lactobacillus organism occurs naturally in fruits and vegetables. Marshall (2010) tested L. Casei among other beneficial probiotics to assess their readiness to fight pathogenic organisms in case of invasion and found that these small pieces of RNA or ORNs control the expression of growth genes in the pathogen’s genomes. The bacteria grow faster after releasing the ORNs, mounting a better defense system to invading bacterial infections (Marshall, 2014).
MicroRNA (or ORNs) play important regulatory role in physiological processes in animals (and plants), and is studied for miRNA-based therapeutics (Wahid et al., 2010). miRNA regulate gene expression in all aspects of biology, with certain endogenous miRNAs participating in antiviral defense mechanisms, such as miR-32 with inhibitory effects against the retrovirus type 1 (PFV-1; similar to human immunodeficiency virus such as Epstein-Barr and others) and protects human cells from PFV-1 (Lecellier et al., 2005). Other studies, such as Ma et al. (2011) found another miRNA (miR-29) controlling innate and adaptive immune response to intracellular bacterial infection. With dysbiosis of the gut, inflammation hasten immunological imbalances, influencing the onset of many chronic illnesses, including cancer. The opposite is also a viable solution – maintaining the health of the microbiome (Cianci et al., 2019).
Lactobacillus acidophillus and Bifidobacterium bifidum regulate and modulate the GI-tract, increasing production of certain microRNA that improve colon cancer treatment (Heydari et al., 2018). From the GI-tract to the brain, Zhao et al. (2019) have shown that probiotics protect against inflammatory neurodegeneration caused by neurotoxins in the gut, contributing to a healthier brain function. Probiotics with their supernatant and microRNA or ORNs regulate and support a balanced function of the GI-tract. MicroRNA have emerged as major players in the interaction between host (human body) and bacterial pathogens, with an integral part in the host immune response to bacterial infection (Aguilar et al., 2019; Sunkavali et al., 2017).
Read more on supernatant, chronic illnesses and the science of healthy longevity in our No 7 Systemic Booster: The New Longevity, Here.
PREBIOTIC & FIBER
Definition: “A prebiotic is a selectively fermented ingredient that allows specific changes, both in the composition and/or activity in the gastrointestinal microbiota that confers benefits upon host well-being and health” (Tufarelli & Laudadio, 2016; Gibson et al., 2017; 2014; Macfarlane et al., 2006). A prebiotic is a fiber that resists digestion in the upper bowel and ferments easily in the colon by probiotic organisms. Prebiotic fibers are imperative for the survival and success of microorganisms, without adequate amounts of prebiotic fiber, probiotic cannot successfully grow and replicate in the gut (Holscher, 2016). To positively modulate the composition and ecosystem of the gut, fiber, both plant fibers and prebiotic fibers that are designated as ‘prebiotic’ are a must have daily nutritional food (David et al., 2014).
History: In 1995, Gibson & Roberfroid introduced the concept of prebiotic as a useful non-digestible fiber such as oligosaccharides, and in particular, fructo-oligosaccharides. In 2017, the International Scientific Association for Probiotics and Prebiotics (ISAPP) released a consensus statement on the definition of scope of prebiotics: The realization that prebiotic fibers stimulate probiotic bacteria’s growth and ability to replicate successfully, and in turn, a healthy community of probiotics modulates the colon’s microbiota by positively changing the ecosystem balance in the GI Tract (Gibson et al., 2017).
Prebiotic Criteria: Following this consensus, three criteria are required for a prebiotic: 1. That the fiber resists digestion by host (fibers that humans cannot digest in the stomach, such as inulin), 2. that the fiber can be fermented by intestinal microorganisms, and 3. The fibers can stimulate the growth and activity of intestinal bacteria associated with health and well-being (Gibson et al., 2017, p. 492). In other words, adding inulin or other non-digestible fibers to a probiotic formula makes sense. Not only do the fibers help selective organisms grow, a prebiotic also must ‘evoke a net health benefit’ (p. 493). Prebiotics, in fact, activates the bacteria in the gut and improve ‘distant sites’ in the body, such as effecting bone strength, supporting neural and cognitive processes, immune function, skin and more (Collins & Reid, 2016).
Food for Microbes: Human beings cannot digest most complex carbohydrates and plant polysaccharides, but microbes do – they metabolize the polysaccharides into short-chain fatty acids (SCFAs), including butyrate (Holscher, 2017). Delcour et al. (2016) examine the metabolites (or supernatant) formed by digesting the fiber and concluded that prebiotic increases production of SCFAs is a viable link between prebiotic, probiotics and health benefit. SCFAs are shown in research to regulate glucose metabolism and control body weight (Canfora et al., 2015), produce anti-inflammatory properties to calm inflammatory bowel disease (Tedelind et al., 2007; Vinolo et al., 2011).
Studies show that when we combine prebiotics with probiotics, many other health benefits follow, such as, prevention of insulin resistance, prevention of obesity, and reduction of FPG (fasting plasma glucose) and plasma insulin (Beserra et al., 2015; Cerdó et al., 2019; Razmpoosh et al, 2019, respectively), all markers for cardiovascular, diabetes, and weight management and control.
Other substances that regulate gastrointestinal health are the oligosaccharides in human milk, important in the development of the newborn intestinal microbiota, metabolic, and immunological systems, all important for health later in life. Similar to the oligosaccharides in human milk, short-chain galacto-oligosaccharides and long-chain fructo-oligosaccharides have been found to effect early microbiota and increase Bifidobacterium growth, and reduces inflammation in the bowel and skin of babies and the young (Oozeer et al., 2013; Wopereis et al., 2018), reduce weight and inflammatory markers in both young and older individuals (Sahlitin et al., 2019; Fernandes et al., 2017, respectively), and generally contribute to healthy ageing (Tihonen, 2010; Buford, 2017).
Not all dietary fibers are characterized as prebiotics, however, they do contribute positive health effects. For example, microbes are unable to ferment cellulose well, but cellulose increases gut transit time. Psyllium is non-fermentable, yet it is shown to improve glycemic control and reduce cholesterol. Fibers, whether prebiotic or not, are healthy for human health.
Complimentary Products
-
If you get fatigued, flushed, or foggy after eating, HistaHarmony, DAO (Diamine Oxidase) enzyme may...
-
MegaSporeBiotic™ is a 100% spore-based, broad-spectrum probiotic shown to be effective in promoting gut health....
- Select options This product has multiple variants. The options may be chosen on the product page
-
MegaSporeBiotic™ Gummies are a 100% spore-based proprietary probiotic blend that supports a healthy gut microbiome...
-
MegaMucosa is the first complete mucosal support supplement of its kind, formulated to support a...
Reviews