Genetics and Hormone Production, Transport, Utilization, and Metabolism
Our genetics play a larger role in our hormones than

Our genetics play a larger role in our hormones than
Have you wondered why an antidepressant didn’t work for you?
https://vimeo.com/821487331 If you’ve ever bought a detox kit off
Although the brain is what we use to think, it’s often the very last thing that we think of when it comes to improving our health.
However, we understand now more than ever that the brain is so much more than a processing center for thoughts and memories. In fact, if your health were an orchestra, the brain would be the conductor — taking the lead role, and — ideally — making sure that all other parts of the body are keeping time and working in harmony.
In this post, we’ll review:
Thinking caps on — let’s get started.
Note: the information below should not be considered medical advice, and it is only available for educational purposes. You should consult your healthcare provider if you have questions or personal health concerns.
The brain and spinal cord are the two organs that compose your central nervous system. Extending from these two organs are many nerves that reach into the far corners of the body. This network of nerves is your peripheral nervous system, and their purpose is to allow for communication between the central nervous system and the other parts of your body.
The peripheral nervous system can also be further subdivided into the autonomic nervous system and the somatic nervous system. The autonomic nervous system comprise all of the nerves that connect the brain to your internal organs — like your liver, your stomach, your heart, and your small and large intestines. These organs work automatically — you don’t have to think about them which is why it earns the name autonomic.
On the other hand, the somatic nervous system is composed of the nerves that connect to your skeletal muscles — which you consciously direct the movement of. Put simply — you can control your somatic nervous system, but the autonomic nervous system is out of your control. This is a good thing – imagine trying to focus on your work call while needing to manage your heart beating and your intestines digesting your food!
Finally, the nervous system can also be divided into the parasympathetic nervous system and the sympathetic nervous system. The parasympathetic nervous system is the “default” state, one of calmness, recovery, digestion, and optimal health function.
The sympathetic nervous system, on the other hand, is also known as your “fight or flight” response. It activates in response to environmental or internal triggers and causes a number of metabolic and biochemical changes to the body that prioritize survival over optimal health.
In short, if the sympathetic nervous system is “fight or flight,” then the parasympathetic nervous system is “rest and digest.” Having a healthy response from both is actually ideal – we don’t just want to have a good parasympathetic response.
“If your health were an orchestra, the brain would be the conductor — taking the lead role, and — ideally — making sure that all other parts of the body are keeping time and working in harmony.”
Now that we’ve got the basics of the nervous system sorted, how exactly does it communicate with your body?
That’s where neurotransmitters come in. What are neurotransmitters, exactly? They are compounds that relay messages to and from the central nervous system.
You’ve probably heard of several neurotransmitters, including:
These neurotransmitters are made from nutrients in our food and — in the case of dopamine — synthesized in the digestive tract, so gut health plays a surprisingly important role in neurotransmitter production and function. [1]
In addition to neurotransmitters and the structural components of nervous system modes, there are numerous other hormones, compounds, brain structures, and cells that play a role in brain health — and therefore overall wellness. We will touch on some of these briefly in this article and in future pieces on functional neurology.
Your body’s sympathetic “fight or flight” response is meant to be a temporary state that helps you survive stressful, life-threatening situations.
Think about the types of stressors our distant ancestors may have faced. Yes, they had interpersonal issues that may have caused them psychological stress, but their primary stressors included short-term problems such as exposure to the elements, being chased by a predator, injuries or illnesses, or starvation.
These differ hugely from the long-term stressors we face today, like work, financial pressure, social media pressure and even commuting — not to mention the cellular stress our bodies face from modern food, exposure to toxins in household or grooming products, and sedentary lifestyles.
Today, many people may be in a seemingly permanent fight or flight mode due to one or more of these stressors, and that may affect overall health — including brain health. We’ll talk more about this below.
You’ve probably heard the term before, but you may be wondering exactly what a neurodegenerative disease is. According to the U.S. National Library of Medicine, neurodegenerative diseases are caused by the dysfunction and breakdown of nerves. [2]
They can affect various domains of your health — like your balance and ability to move or control your skeletal muscles, talking, ability to communicate, your memory, your perception, or even your breath control and heart function.
They can be genetic, or they can result from environmental triggers such as other medical conditions, viruses, or toxin exposure.
Additionally, lifestyle may play a large component in the development of certain neurodegenerative diseases.
Neurodegenerative diseases and mood disorders are both conditions of the brain and nervous system, but they have several marked differences.
First, as their respective names suggest, neurodegenerative disorders deal with the neurodegeneration — or the breakdown of brain cells and tissues resulting in memory issues, cognitive changes, and mood disorders (as a symptom of disease progression).
On the other hand, mood disorders — while they may be associated with some level of dysfunction in the cells — typically don’t involve memory loss, loss of coordination or muscle control, or decreases in cognitive function — only changes in mood.
Some research suggests that mood disorders may increase your risk of developing a neurodegenerative disorder in the future, and mood disorders may also arise as a symptom or complication of neurodegenerative disorder. [3]
Three of the most common on the list of neurodegenerative diseases are dementia, Alzheimer’s disease, and Parkinson’s disease. Although these conditions have come to be a widely accepted part of aging, they are all preventable — but until recently, we didn’t really have a good understanding of what lifestyle factors contributed to their development.
These conditions are all thought to arise — at least in part — as a result of neuroinflammation, or brain inflammation. Here’s a bit more about each. [4]
Dementia isn’t actually a disease itself, but instead refers to cognitive changes that make it difficult to function normally. It typically affects older people. Dementia can differ from person to person because there’s no official definition or diagnostic criteria, but may include:
Alzheimer’s is the most common type of dementia, and it is a diagnosable medical condition. Alzheimer’s is considered progressive and irreversible and is divided up into three distinct phases. [5]
The pre-clinical phase of Alzheimer’s, which is symptomless but reflects the brain changes that will eventually cause dementia, highlights just how important it is to focus on early prevention.
Parkinson’s is another common neurodegenerative disease, but unlike dementia it affects movement rather than cognition.
It’s characterized by a gradual loss of muscle control.
People with Parkinson’s may first develop tremors in their hands, but the disease can eventually progress to a complete loss of ability to speak or stand. Additionally, many people with advanced stages of Parkinson’s also have dementia. [6]
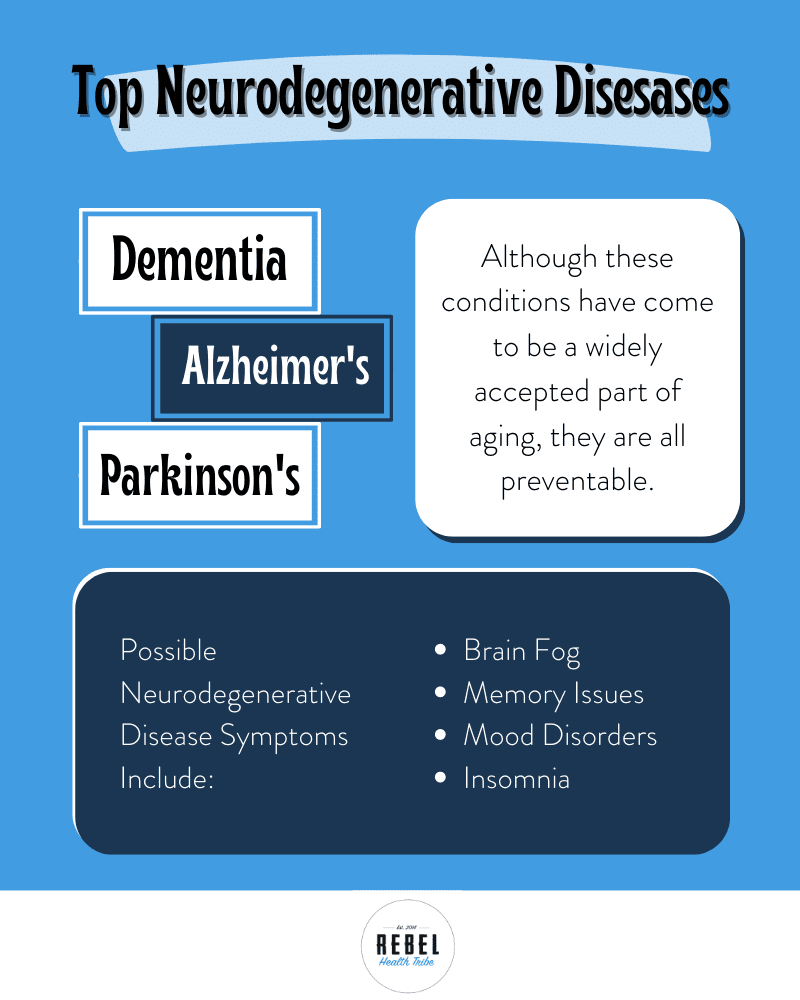
The brain inflammation symptoms below are signs that your brain may not be functioning optimally. They can be indicators of neurodegenerative disease, as well.
Brain fog is hard to describe, but it is essentially a groggy, hazy feeling that limits your ability to focus or be productive. In research, the term brain fog is generally interchangeable with mental fatigue. [7]
Memory loss is often the first major indicator of neurological disease. In early stages of Alzheimer’s, memory loss occurs because neurons — brain cells — lose their ability to communicate effectively with one another, but as the disease progresses memory loss may be due to cell death and loss of structures in the brain. [8]
Mood disorders such as depression and bipolar disorder are signs that there may be some dysregulation in your brain. In people with neurological diseases, mood disorders are often seen as well.
With insomnia, you may commonly have long nights where you have trouble going to sleep. Since sleep is absolutely vital for brain health, rest, and healing — over time constant lack of sleep may lead to more serious brain and health issues.
In addition to these neurodegenerative disorders, there is another class of disorder that may affect the nervous system as well. Autoimmune disorders arise when the body’s immune system launches an attack against its own healthy cells or organs. Autoimmune disorders can affect any organ or body part, but there are several that may focus on the brain or nervous system.
One example is multiple sclerosis, in which the immune system attacks the linings of nerve cells. This can cause a huge variety of symptoms that may include poor coordination, vision changes, and fatigue.
Another example is pediatric autoimmune neuropsychiatric disorder associated with streptococcal infections (PANDAS) — this autoimmune disorder occurs in children after the immune system attacks healthy cells that resemble strep bacteria. [9]
However, the full neurological autoimmune disease list is much longer.
There are several other nervous system disorders that don’t fit these categories as well.
Childhood neurological diseases include autism spectrum disorder and attention deficit disorder (ADD/ADHD).
Anxiety affects millions of people in the U.S. — approximately 18% of the population. [10]
Traumatic brain injury, post-traumatic stress disorder (PTSD), and addiction can also profoundly affect brain function and brain chemistry as well as the physical structures of the brain.
There’s an entire emerging branch of medicine — called psychoneuroimmunology — dedicated to the interplay between neurological health, immunity, and the endocrine (hormone) system.
Like all other body systems, the health of your brain and nervous system is intricately and intrinsically connected to the health of every other part of your body. The importance of the brain’s contribution to health or disease can’t be overstated.
Here are a few important ways that the nervous system may contribute to health or disease.
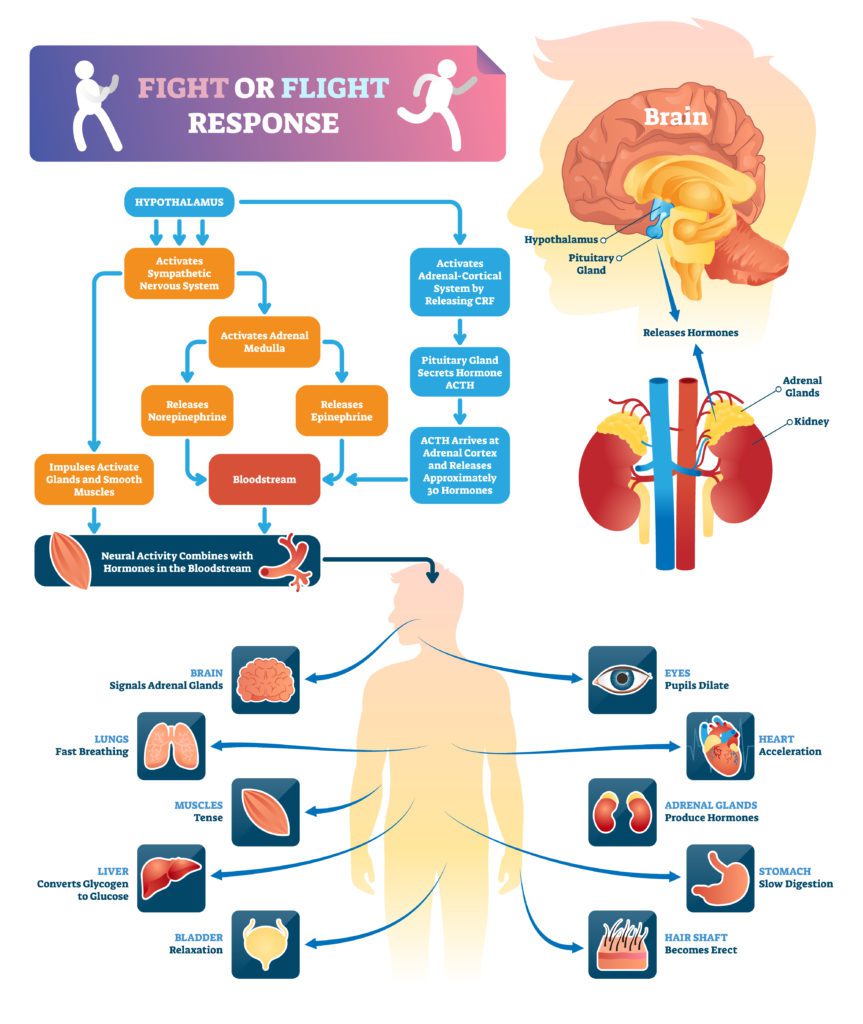
If you’re feeling stressed out (and who’s not these days?), you may be in fight or flight mode… and you may have been in that mode for a long time.
When your body’s sympathetic nervous system is activated, every bodily process shifts to survival. You may have elevated stress hormones, like cortisol — which will promote abdominal fat storage (providing stored energy for protection against starvation, which probably isn’t what has you feeling stressed).
You may not sleep well, and you may crave higher-calorie foods. These behaviors used to be protective, but the fight or flight response hasn’t quite caught up to our modern lifestyles yet. [11]
You may also experience chronic, systemic inflammation — which is an immune response to stress that plays a major role in the development of other chronic conditions, like autoimmune disorders, type 2 diabetes, and heart disease. This can include inflammation of the brain.
Mood disorders like depression, anxiety, and bipolar disorder are thought to affect about 20% of the population at some point in their lives, although many researchers suspect that these rates have increased sharply in the aftermath of the COVID-19 pandemic. [12]
These mood disorders have been linked to lifestyle factors like sugar intake, lack of exercise, and poor sleep.
And regardless of which came first — the lifestyle changes or the mood disorder — it does look like these lifestyle factors can further exacerbate mood disorders. They may also promote inflammation, which can keep your fight or flight response activated. Likewise, these lifestyle behaviors may also introduce large amounts of free radical compounds, which can cause cellular dysfunction.
Another consideration is the microbiome. Researchers have found that the composition of the gut microbiome plays a major role in mood regulation, particularly since dopamine — the pleasure hormone — is produced in the gut as a byproduct of bacterial metabolism. [13]
Your diet and lifestyle can also profoundly affect your microbiome, so some changes to these factors can majorly affect your overall health — both physical and mental.
The vagus nerve is a major nerve that innervates the digestive system. It also plays a key role in the activation and regulation of the parasympathetic nervous system.
Vagal tone refers to how responsive your vagus nerve is. In people who are in a continuous state of fight or flight, the vagus nerve may be poorly responsive. However, there are several ways you can improve vagal tone and help your body switch back into “rest and digest” mode. (We’ll dive into those in the next sections.) [14]
As you may already be able to tell, none of these issues exist in a vacuum — they all overlap and feed on one another. Stress may cause you to be in fight or flight mode, which may cause you to sleep poorly and make poor food choices. Then you probably don’t feel like working out, and your mental health may suffer — further decreasing your motivation.
And this is just one example of the snowball effect of fatigue, depression, brain fog, low motivation, low activity, and poor dietary choices that can make it really, really hard to make positive changes for your health. However, taking small steps to improve in these areas can make a big difference for your overall health and your brain health.
Here are some of the key factors that may affect your brain and nervous system health.
Chronic neuroinflammation is one of the main drivers of brain and nervous system dysfunction, from mood disorders to degenerative brain diseases.[15][16]
This chronic inflammation can be caused by numerous factors, including poor diet, chronic stress, exposure to toxins, molds, or heavy metals, inadequate sleep, and more.
Traumatic events and chronic mental stress can shift your body into a semi-permanent fight or flight mode. As we’ve discussed at several points above, this continuous activation of the sympathetic nervous system can be devastating for your overall health — including your brain.
Although it can be difficult to address these issues, they must be addressed for you to make progress and to truly and permanently improve your health. Improving your vagal tone can help your body to shift back into “rest and digest” mode.
A diet high in added sugars, refined seed oils, and processed foods can also contribute to systemic inflammation in a significant way. [17][18][19]
Likewise, we are meant to move and spend time outdoors — so being indoors and sedentary can put a lot of extra stress on your body not just physically but all the way down to a cellular level. [20]
You can make diet and exercise work in your favor by being active regularly, spending more time outdoors, and choosing a healthy diet of minimally processed whole foods – literal brain food.
Blood sugar imbalances can also contribute to neurological dysfunction. In research and medical circles, Alzheimer’s disease is known as type 3 diabetes and described as “insulin resistance of the brain.” [21]
When your blood sugar levels are consistently high, your body may begin to ignore the hormone insulin — which leads to high insulin levels. These high insulin levels are linked to weight gain, inflammation, high blood pressure, heart disease, and — yes — neurological changes. [22]
Can dementia be reversed? It may not be possible to completely reverse a neurodegenerative brain disease once it’s reached a point where it’s diagnosable, but some researchers have made great strides in developing neuroinflammation-reducing protocols that may help to drastically reduce symptoms and improve quality of life. For example:
You can learn more about these researchers and their protocols in our Brain and Nervous System Masterclass.
Because it may not be possible to completely reverse neurological disease, it’s important to adopt a lifestyle that promotes neurological health and regulating the nervous system as early as possible to help prevent these conditions and optimize your brain health.
But how do you prevent dementia naturally? Fortunately, a brain-healthy lifestyle is one that is nourishing and healthy for the rest of your body (and your mental health) as well. Natural ways to improve your brain health and related health conditions include:
Bottom line, brain health can be extremely complicated. We have just barely scratched the surface of the basics of brain and nervous system health in science but we are constantly learning more. Our goal is to keep you informed of the latest research through solid content to help you optimize your cognition and mood. But this much we know is true – rest assured that a lifestyle that’s good for your body is good for your brain, too.
If you get fatigued, flushed, or foggy after eating, HistaHarmony,...

MegaSporeBiotic™ is a 100% spore-based, broad-spectrum probiotic shown to be...
MegaSporeBiotic™ Gummies are a 100% spore-based proprietary probiotic blend that...
MegaMucosa is the first complete mucosal support supplement of its...
An Exclusive Course with 10 Years of Microbiome
If you’ve ever wanted all of Kiran’s best
The toxicity and Detoxification Masterclass covers a wide
19 Leading Experts Share Cutting-Edge Science, Effective Practices,
Autoimmune Masterclass brings together 17 of the world’s
If you get fatigued, flushed, or foggy after...

MegaSporeBiotic™ is a 100% spore-based, broad-spectrum probiotic shown...
MegaSporeBiotic™ Gummies are a 100% spore-based proprietary probiotic...
MegaMucosa is the first complete mucosal support supplement...
An Exclusive Course with 10 Years of Microbiome Knowledge Build Your Resilient Gut: Microbiome & Beyond with Kiran Krishnan is the
If you’ve ever wanted all of Kiran’s best content in one place, here they are! These are the exact trainings
The toxicity and Detoxification Masterclass covers a wide array of topics with the following guests: 1. Lara Adler, Environmental Toxins
19 Leading Experts Share Cutting-Edge Science, Effective Practices, and Clinical Strategies to Optimize Brain & Nervous System Health in Kids