
Meet Your Microbiome: The Human Microbiome and How to Optimize It
Meet Your Microbiome: The Human Microbiome and How to Optimize

Meet Your Microbiome: The Human Microbiome and How to Optimize

Benefits of Probiotics Including Improved Gut Health “Probiotics” has become
Gut Microbiome Health and the Gut-Immune System Connection: Part 2
The message is out: gut health is critical for wellness. Everywhere you look, you’ll see headlines about a new study about the microbiome. From cardiovascular disease to autoimmunity, our gut bugs are involved in all aspects of health.
The relationship is complex, and there’s still so much to learn, but it’s clear that we’ve evolved to work in harmony with our microbes. When it’s healthy, your gut is a hub of activity that helps you digest food, absorb nutrients, and activate your immune system. But when the microbiome is altered, it can lead to significant health consequences.
To understand the scope of all the microbiome does, let’s take a journey through the digestive tract. From the first bite of food to the moment of elimination at the other end, the microbiome is at work promoting optimal health.
In this article, we’ll provide a comprehensive overview of the upper GI tract with a focus on the microbiome and its unique role in digestion. We’ll cover:
Let’s start with the human gut microbiome to better understand its importance and relevance to health. The microbiome refers to the trillions of microorganisms that live in and on our bodies. We’ve evolved to coexist with these creatures beyond simply saying they benefit our health. We live symbiotically with our microbiome, where they are actually imperative for our wellbeing. This community of microbes helps us digest food, synthesize vitamins and minerals, and protect us from harmful pathogens.
Our diet and digestive process impact our gut microbiome, but the presence or absence of microbes can also alter digestion efficiency. Let’s look at the organs of the upper digestive system and how it all works together and interacts with your microbiome.
Before you even open your mouth to that first bite, your digestion is already gearing up. Just the thought of food leads to the secretion of salivary enzymes like amylase, an enzyme that breaks down starches. When you see and smell an enticing meal, your body essentially primes the engine, preparing you for the next step.
Once the saliva is flowing, it’s time for your first bite. Chewing is the next essential act of digestion. As you chomp and grind food particles, you prepare them to pass through the digestive system at a more manageable size.
“Your mouth is where digestion starts, and the microbiome in your mouth influences everything that comes next.”
All those times your parents told you to chew your food? They were absolutely right. The more you chew, the easier your food is to digest.
Now, that doesn’t mean all those times you scarfed down your dinner meant you didn’t digest it. Your digestive system is pretty impressive and all those enzymes and acids will eventually break down pretty much anything you ingest. But chewing has several important functions:
Saliva is secreted by specialized glands in your mouth. Made up of water, enzymes, electrolytes, and mucus, saliva is essential for a healthy mouth and smooth digestion.
Your mouth requires a certain amount of saliva at all times for optimal oral health. However, signals from your nervous system cause the release of higher amounts of saliva when you eat. Here’s why:
While much of the focus of the microbiome is on the lower part of your digestive tract, you also have an oral microbiome. Your mouth contains the second-highest number of microorganisms after your intestines. The oral microbiome exists as a biofilm that covers the mucosa of the mouth and the teeth.
This microbiome maintains the health of your teeth, gums, and mouth. Microbes from the oral microbiome travel to other parts of the body, impact the health of the gut, and can even alter the immune system.
If the balance of microorganisms in your mouth is disrupted, the effects can be far-reaching. Microbes from the mouth have even been implicated in conditions such as small intestinal bacterial overgrowth (SIBO) where the small intestine is overtaken by harmful bacteria. If harmful bacteria gain a foothold in your mouth, they may decide to travel, putting the rest of your GI system at risk.
Our Deep Dive: SIBO webinar is a helpful resource for understanding the link between the oral microbiome and SIBO.
A balanced oral microbiome aids digestion, converts nitrate from fruits and vegetables into nitrite (important for blood pressure regulation), and protects the mouth from oral diseases. If the microbiome of the mouth is imbalanced, it may lead to conditions such as gingivitis, infections, cavities, and even chronic diseases such as heart disease, stroke, diabetes, and systemic inflammation.
A combination of factors influences the microbes that thrive in the oral environment. Things such as:
Your mouth is where digestion starts, and the microbiome in your mouth influences everything that comes next.
“From the first bite of food to the moment of elimination at the other end, the microbiome is at work promoting optimal health.”
As food leaves your mouth, peristalsis (wave-like contractions that push the food down your digestive tract) moves the food down through the esophagus and into your stomach.
Peristalsis breaks down the food into chyme, a mash of partially digested food and gastric juices. Hydrochloric acid (HCl) from your stomach cells plus pepsin, an enzyme needed to break down proteins, get to work.
The acidic environment in the stomach is hostile to harmful pathogens, so it helps protect you from infection. Think of your stomach acid as a gastric barrier that protects you against potential pathogens from the outside world such as bacteria in your food for example. Essentially, healthy stomach acid levels are the gatekeeper that prevents harmful bacteria from entering your small intestine.
The strength of your microbiome relies on healthy amounts of stomach acid. Unfortunately, issues with stomach acid are common. Occasional acid reflux happens to all of us, but an estimated 20% of adults have GERD.
Acid reflux occurs when the stomach contents flow back up into the esophagus. Imagine the very acidic stomach acid entering the tender tissue of your esophagus. Ouch!
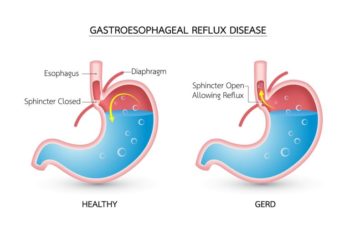
Common acid reflux symptoms include:
GERD is acid reflux that happens so regularly your esophagus becomes damaged. In addition to all normal acid reflux symptoms, GERD symptoms go a step further.
While acid reflux and GERD are typically treated with proton pump inhibitors, a type of medication that reduces stomach acid, it doesn’t always work. Up to 42% of people with GERD don’t respond to medications.
Dropping the pH of the stomach is a questionable solution to acid reflux. It can lead to hypochlorhydria or low stomach acid, which causes problems digesting food and absorbing nutrients. It can also lead to the overgrowth of unfriendly bacteria and yeast. Remember, your stomach acid protects you against unwanted bacteria or other potential pathogens.
Acid reflux and GERD may be a symptom of dysbiosis, or in some cases, it may be a cause. Often our efforts to reduce stomach acid disrupt the balance of the microbiome. Acid reflux is a well-known symptom of dysbiosis. Treatment for GERD needs to honor this complexity and focus on repairing the microbiome and normalizing stomach acid.
Our Microbiome Masterclass lays out step-by-step how to heal your microbiome. Here are a few highlights to get you started.
Diet
What you eat is one of the primary influencers of the health of your microbiome.
Lifestyle
Supplements
Probiotics and prebiotics are powerful support for the microbiome. As you work to restore healthy bacteria, these two supplements may help:
“While a lot of emphasis is placed on the problems that come with too much stomach acid, too little can be just as problematic.”
While a lot of emphasis is placed on the problems that come with too much stomach acid, too little can be just as problematic. Hypochlorhydria is a condition in which too little hydrochloric acid is released. Digestion requires stomach acid to break down food and prepare it for absorption in the intestines. If acid levels are too low, healthy digestion is compromised.
As we’ve mentioned, stomach acid is a key player in protecting the microbiome of the intestines. Too little acid spells disaster for healthy bacteria.
Common causes of low stomach acid include:
To address low stomach acid a few strategies can help:
Eat a nutrient-dense diet
Vitamins and minerals are critical not only for the production of stomach acid, but so many other digestive and body functions. It’s not uncommon for individuals in the modern world to be overfed, but undernourished. Diets high in plant foods provide the best protection against vitamin and mineral deficiency.
Manage stress
Meal time should be a relaxing, nourishing experience. For optimal digestion, set the stage by unplugging from electronics and being a mindful eater. Enjoying meals with others can be one way to lower your stress level and promote healthy digestion.
Consider supplemental hydrochloric acid (HCL)
Some people may benefit from a supplement that provides HCL. HCL Guard™ is a good example of a supplement that boosts HCL levels and also supports healthy digestion with an herbal blend as well as well as intrinsic factor for vitamin B12 absorption.
Gastritis is similar to GERD as the mucosa is irritated, but it’s located in the stomach instead of the esophagus. It’s often caused by Helicobacter Pylori (H. pylori), a commensal organism (meaning we all have it). Many people don’t experience any symptoms from H. Pylori, but if there’s an overgrowth, it can cause a wide range of symptoms, including nausea, vomiting, diarrhea, and abdominal pain.
The gut microbiome plays a role in developing this overgrowth because of the immune system connection. This means dysbiosis can increase the risk of developing gastritis, as does having low stomach acid (even though antacids are often the first-line treatment). On the other hand, H. pylori can increase inflammation and change the balance of the gut microbiome.
Treatment for gastritis typically involves antibiotics to kill the bacteria, but once again, this can often lead to an overgrowth of not-so-friendly bacteria. Taking probiotics as part of the treatment plan may improve outcomes and reduce the incidence of side effects from medications.
A few supplements that can help include:
To round out our walk through the upper GI system, let’s take a look at how the liver and gallbladder contribute to the digestive process.
The liver is the second largest organ in the body (after the skin). It resides in the upper abdomen beneath the diaphragm. In addition to its many essential functions, the liver produces bile to aid digestion.
When you eat a meal, the liver sends bile through the common bile duct into the first part of the small intestine. Between meals, the bile produced by the liver is shuttled to the gallbladder for storage until your next meal.
The gallbladder is a small organ that holds and concentrates bile. When you eat a fatty meal, signals from digestive hormones and the parasympathetic nervous system cause the gallbladder to contract and send concentrated bile down the common bile duct into the small intestine. There bile from both the liver and the gallbladder mix with the chyme from the stomach to further the digestive process.
Bile contains bile salts that break down fat into smaller globules which are easier to digest. However, fat digestion is not its only purpose.
Absorption: The bile salts in bile aid the absorption of essential nutrients such as iron, calcium, and fat-soluble vitamins A, D, E, and K.
Excretion: The liver uses bile as a medium for the excretion of metals, toxins, waste products, and cholesterol. These substances travel with bile through the intestines and become part of feces.
Neutralizer: Bile neutralizes the contents entering the small intestine from the highly acidic stomach. It contains alkali that balances the hydrochloric acid from the stomach.
Anti-microbial: Due to its ability to dissolve fat, bile degrades the integrity of the cell walls of any pathogenic bacteria that enter the digestive system via food. This action protects the body from harmful microorganisms.
The free flow of bile is critical for digestive and overall health. Anything that disrupts bile flow can cause a host of issues.
Cholestasis is a condition in which bile flow is slowed or blocked. This can occur for a variety of reasons.
Symptoms may include:
Anytime there are issues with bile production or flow, two conditions may be worth investigating.
Non-alcoholic Fatty Liver Disease
Non-alcoholic fatty liver disease (NAFLD) occurs when fat deposits build up in the liver. This buildup of fat is usually the result of unhealthy lifestyle habits such as poor diet and lack of exercise, leading to obesity and insulin resistance. Over time, the build-up of fat results in liver dysfunction, potentially impacting bile production.
Small Intestine Bacterial Overgrowth
Understanding bile function makes it easy to see how cholestasis may cause small intestine bacterial overgrowth (SIBO). Without the antimicrobial actions of bile, harmful bacteria can gain a foothold in the intestines.
We’ll cover SIBO in-depth in Part 2 of this series. Our Deep Dive Training: SIBO is also a great resource for learning how bile dysfunction contributes to this condition.
Caring for the liver, supporting the microbiome, and living an overall healthy lifestyle create conditions favorable to optimal digestion and bile flow. A few specific tools to support the liver include:
As you can see walking through the upper digestive tract, how well your gut functions impacts everything. The upper digestive tract not only begins the process of digestion but also lays the groundwork for the health of the microbiome and its impact on whole body wellness.
Optimal digestion begins in the upper digestive system. But, it doesn’t stop there.
Check out Part 2 of this series to continue the tour through the digestive system and the amazing microbiome.
ZenBiome™ Sleep is formulated to help clients deal with occasional...
An Exclusive Course with 10 Years of Microbiome
If you’ve ever wanted all of Kiran’s best
The toxicity and Detoxification Masterclass covers a wide
19 Leading Experts Share Cutting-Edge Science, Effective Practices,
Autoimmune Masterclass brings together 17 of the world’s
If you get fatigued, flushed, or foggy after...

MegaSporeBiotic™ is a 100% spore-based, broad-spectrum probiotic shown...
MegaSporeBiotic™ Gummies are a 100% spore-based proprietary probiotic...
MegaMucosa is the first complete mucosal support supplement...

Meet Your Microbiome: The Human Microbiome and How to Optimize It On and in the average human, there reside approximately

Benefits of Probiotics Including Improved Gut Health “Probiotics” has become quite the buzzword – with countless products and supplements proudly
Gut Microbiome Health and the Gut-Immune System Connection: Part 2 Lower GI The diverse community of microbes in your digestive
Gut Microbiome Health and the Gut-Immune System Connection: Part 1 Upper GI The message is out: gut health is critical